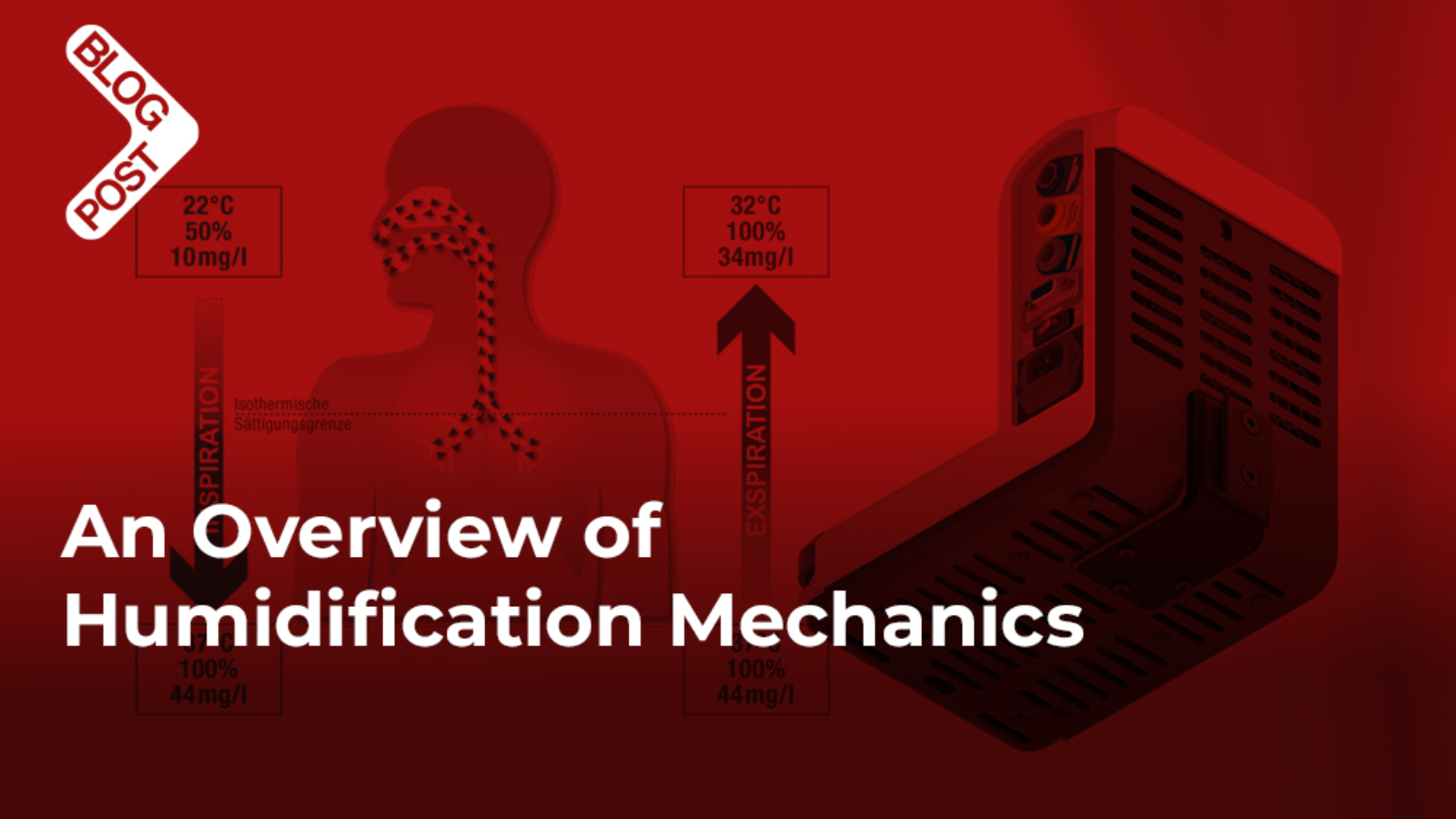
Humidification plays a pivotal role in respiratory care, especially within the context of mechanical ventilation. Ensuring optimal humidity levels is essential not only for patient comfort but also for safeguarding the respiratory tract and enhancing ventilation outcomes. The mechanics behind effective humidification are designed to mimic natural airway conditions, compensating for the absence of the upper airway’s natural humidifying functions. Understanding these mechanics helps clarify why maintaining ideal humidity levels is so critical for both acute and long-term respiratory support.
Importance of Humidification in Ventilation
Humidification is critical in mechanical ventilation for several physiological reasons. First, it prevents the drying and damage of airways. When gases are delivered during mechanical ventilation, they bypass the upper respiratory tract, which naturally warms and humidifies air. Without humidification, the cold and dry gas can dry out airways, leading to discomfort, irritation, and potential damage to the mucosal lining (1,2). This prolonged exposure can cause secretions to thicken and increase the risk of airway blockage.
Second, humidification is vital for maintaining mucociliary function. The respiratory system’s mucociliary escalator relies on a well-hydrated mucus layer to trap and remove particles and pathogens. Adequate humidity keeps the mucus moist, allowing cilia to move it effectively out of the airways. In contrast, without sufficient humidity, mucus thickens, resulting in secretion retention and a heightened risk of infection (3).
Moreover, proper humidification reduces the risk of atelectasis, where mucus plugging obstructs the airways and compromises lung function. By preventing thick secretions, humidification helps maintain open airways, optimizing ventilation and oxygenation. It also aids thermoregulation by minimizing water and heat loss through the respiratory tract, thus preventing hypothermia and dehydration, especially in patients requiring prolonged ventilation.

Enhancing Patient Comfort and Breathing Efficiency
Humidified gases enhance patient comfort by preventing dryness in the mouth, nose, and throat, which is crucial for those on long-term ventilation. Furthermore, it reduces the risk of respiratory infections by maintaining moisture in the airways, promoting pathogen clearance, and minimizing the formation of stagnant mucus, which can harbor bacteria (4).
Finally, properly humidified air decreases airway resistance, easing the effort required for breathing. This is particularly important for critically ill patients or those on ventilators, as it facilitates better gas exchange and reduces the work of breathing (5,6).
In summary, humidification is essential to maintaining respiratory function, protecting the airways, and enhancing the overall outcomes of mechanical ventilation. It significantly improves patient comfort and reduces the risks of complications associated with long-term ventilator use.
Overview of Humidifiers and Ventilators
Mechanical ventilation and humidification are essential components in respiratory care, particularly for patients requiring long-term respiratory support. Ventilators deliver oxygen to patients, and humidifiers are used to ensure that the air provided is moistened and warmed, simulating the natural humidification process of the human body (7-10).
Types of Humidifiers for Ventilators
Humidifiers used in ventilation fall into two categories: heated humidifiers, which actively heat and moisten the air delivered by the ventilator, and heat and moisture exchangers (HMEs), which capture moisture and heat from exhaled air for reuse during inhalation.
- Heated Humidifiers (Active Humidification)
- These devices actively heat and add moisture to the air delivered by the ventilator, providing optimal humidification levels.
- Heat and Moisture Exchangers (Passive Humidification)
- Also called “artificial noses,” these devices trap the moisture and heat from the exhaled air and reuse it during the next inhalation, offering an easier and less energy-invasive method of humidification.
Heated Humidifiers
Heated humidifiers are devices designed to add moisture and warmth to the air delivered by mechanical ventilators to patients. This is essential because mechanical ventilation bypasses the body’s natural mechanisms for humidifying and warming air, which are usually done by the nose and upper airways. Without proper humidification, dry, cold air can irritate and damage the respiratory tract.

Key Components of Heated Humidifiers:
- Water Reservoir/Chamber:
- Contains water that is heated to generate moisture.
- Heater Element/Heated Plate:
- Located under the water reservoir, it heats the water to produce warm, humidified air. The heating element can be adjusted to achieve the desired temperature and humidity level.
- Temperature Sensors:
- Sensors monitor the temperature of the gas at the humidifier outlet and adjust the heating to ensure optimal humidification and prevent overheating.
- Heated Wire Circuit:
- The ventilator circuit (tubing) often includes heated wires that help maintain the temperature of the humidified gas as it travels through the tubing to the patient, preventing condensation (rainout).
- Control System:
- Modern humidifiers are equipped with control units that regulate temperature and humidity based on patient needs, ensuring precise control over the humidification process.
How Heated Humidifiers Work:
Heated humidifiers work by heating water in a chamber to create water vapor, which is then mixed with the gas flow from the ventilator. As the gas passes over the heated water, it picks up both moisture and heat. This warm, humidified gas is delivered through the ventilator circuit to the patient’s lungs, with heated wires in the tubing helping to maintain the temperature and moisture content along the way.
This ensures that the gas remains at an optimal level for the patient’s comfort and respiratory health. The temperature at the airway is typically regulated around 37°C, mimicking body temperature, to prevent cooling and condensation in the tubing. The humidifier continuously adjusts its heating to strike the right balance between temperature and moisture for effective respiratory care (11-13).

Benefits of Heated Humidifiers:
Heated humidifiers offer several key benefits in respiratory care. They prevent the drying of airways, which can lead to irritation, excessive mucus production, and airway obstruction. By providing proper humidification, they help keep mucus thin and mobile, reducing the risk of mucus plugging that could result in atelectasis (lung collapse) or infection.
Heated humidifiers also maintain body temperature by delivering air that matches the body’s natural warmth, minimizing the risk of hypothermia, which is crucial for critically ill patients or those on long-term ventilation. Additionally, they enhance gas exchange by supporting the normal function of the lungs and respiratory system, leading to improved oxygenation and ventilation. Finally, they significantly improve patient comfort by delivering warm, moist air, preventing dryness and irritation in the airways (11-13).
Applications of Heated Humidifiers:
- Invasive Mechanical Ventilation:
- Heated humidifiers are commonly used in patients on invasive mechanical ventilation, such as those with endotracheal or tracheostomy tubes. These devices bypass the upper airway, eliminating the natural humidification processes of the body (12).
- Non-Invasive Ventilation (NIV):
- In non-invasive ventilation, such as Continuous Positive Airway Pressure (CPAP) or Bi-level Positive Airway Pressure (BiPAP), heated humidifiers are often used to enhance comfort and maintain airway moisture (12).
Challenges and Considerations:
- Condensation (Rainout):
- One of the common challenges is condensation within the ventilator tubing, which can occur when the humidified air cools down as it travels through the circuit. This “rainout” can lead to water accumulation in the tubing, which may disrupt ventilation and increase the risk of infection. Heated wires in the circuit help mitigate this issue by maintaining a constant temperature.
- Infection Risk:
- Heated humidifiers require regular cleaning and maintenance to prevent bacterial growth in the water reservoir. The use of sterile or distilled water is crucial to minimize the risk of contamination.
- Energy Consumption:
- Heated humidifiers require electrical power to maintain the heating element, making them more energy-dependent than other forms of humidification like heat and moisture exchangers (HMEs).
- Monitoring and Adjustment:
- Regular monitoring is needed to ensure that the humidity and temperature are set at appropriate levels, tailored to the patient’s needs (17-21).
Comparison with Other Humidification Methods:
- Heat and Moisture Exchangers (HME):
- Unlike heated humidifiers, HMEs are passive devices that trap moisture and heat from the patient’s exhaled air and return it during inhalation. While they are simpler and do not require power, HMEs are less effective in long-term ventilation or for patients with high minute ventilation.
In conclusion, heated humidifiers are essential for ensuring optimal humidification and temperature control in mechanically ventilated patients, especially in critical care settings. Their ability to provide warm, moist air helps prevent complications associated with dry airways, improves patient outcomes, and enhances overall comfort.
Heat and Moisture Exchangers (HMEs)
Heat and Moisture Exchangers (HMEs), also known as “artificial noses,” are passive devices used in respiratory care to conserve moisture and heat in the breathing circuit of mechanically ventilated patients. Unlike active humidifiers, which add heat and water vapor to the air, HMEs capture and reuse the patient’s own exhaled heat and moisture to humidify the inhaled air.

Key Components of HMEs:
- Core (Moisture Retaining Material):
- The core of the HME is made of hygroscopic material (e.g., paper or foam) coated with salt or other substances that retain moisture and heat.
- Filter:
- Some HMEs include a bacterial or viral filter to trap pathogens, offering additional protection against infections.
- Housing:
- The outer shell is typically plastic and designed to fit into the ventilator circuit. It connects between the endotracheal tube or tracheostomy tube and the ventilator tubing.
How HMEs Work:
During Exhalation the warm, moist air passes through the HME. The hygroscopic material in the HME absorbs moisture and retains the heat from the exhaled air.
During Inhalation the air passes back through the HME. The retained moisture and heat from the exhaled air are transferred to the cool, dry inhaled air, warming and humidifying it before it reaches the lungs.
This cycle repeats with every breath, continuously maintaining humidity and temperature within the respiratory system (23).

Types of Heat and Moisture Exchangers (HMEs):
- Simple HME:
- These HMEs passively trap heat and moisture from exhaled air without any active warming or humidification. They are inexpensive and widely used in short-term ventilation.
- Hygroscopic HME:
- These HMEs use special materials, such as calcium chloride, which enhance moisture retention from exhaled air. They offer better humidification compared to simple HMEs.
- Hydrophobic HME:
- Made from water-repellent materials, these HMEs focus on capturing heat rather than moisture. They also help reduce bacterial contamination by acting as a filter.
- HME with Integrated Filters:
- These devices incorporate bacterial/viral filters to trap pathogens, offering a dual function of humidification and infection prevention.
Benefits of Heat and Moisture Exchangers:
Heat and Moisture Exchangers (HMEs) offer several benefits, particularly in terms of simplicity and convenience. They are easy to use, disposable, and require no power source or complex setup, making them ideal for short-term or emergency ventilation situations. HMEs are also cost-effective compared to heated humidifiers, with less need for maintenance, which makes them suitable for temporary or non-invasive ventilation.
Additionally, because they are single-use devices, HMEs reduce the risk of cross-contamination and eliminate the need for continuous cleaning and sterilization, unlike heated humidifiers that require regular disinfection. Their lightweight and portable design also makes them highly practical for non-invasive ventilation (NIV) and patient transport scenarios (24).
Limitations of HMEs:
Heat and Moisture Exchangers (HMEs) have several limitations, particularly in high-demand respiratory situations. Their efficiency decreases in patients with high minute ventilation, where large volumes of air need to be humidified. This can lead to airway dryness, mucus plugging, and lung complications. Additionally, excess moisture can cause the HME to become saturated, resulting in increased resistance, potential blockage, and reduced effectiveness in delivering humidified air.
HMEs are generally intended for short-term use, typically up to 48 hours, making them less suitable for long-term ventilation where heated humidifiers are more effective. They also add a small amount of dead space to the ventilator circuit, which can increase the work of breathing, especially in pediatric or neonatal patients.
Furthermore, HMEs are less effective in certain clinical situations, such as with patients who have thick or copious secretions, and are not recommended for those requiring high levels of humidity or oxygen, such as patients on high-flow oxygen therapy (23-25).
Applications of HMEs:
- Invasive Mechanical Ventilation:
- HMEs are commonly used in patients on invasive ventilation, particularly those who require short-term ventilation in settings like the operating room, recovery rooms, or emergency departments.
- Non-Invasive Ventilation (NIV):
- HMEs are also used with NIV devices such as Continuous Positive Airway Pressure (CPAP) or Bi-level Positive Airway Pressure (BiPAP) systems. They help improve comfort and maintain airway moisture in patients using masks for ventilation.
- Post-Surgical Care:
- In post-operative settings, HMEs are useful in maintaining airway moisture for patients recovering from surgeries, especially in cases where mechanical ventilation is required for short periods.
- Home Care and Transport:
- HMEs are favored in home care settings for patients on ventilators due to their simplicity and low maintenance. They are also commonly used during patient transport, where active humidifiers may not be feasible.
Comparison Between HMEs and Heated Humidifiers:
| Aspect | Heat and Moisture Exchanger (HME) | Heated Humidifier |
| Mechanism | Passively conserves moisture and heat | Actively adds moisture and heat |
| Power Requirement | No power required | Requires electrical power |
| Humidity Control | Less precise; relies on patient exhalation | Precise control over humidity and temperature |
| Efficiency | Less effective in high minute ventilation | Highly effective for long-term ventilation |
| Cost | Low, disposable | Higher cost, requires regular maintenance |
| Infection Control | Single-use, minimizes contamination | Needs regular cleaning to prevent infection |
| Applications | Short-term, low-risk ventilation | Long-term ventilation, critically ill patients |
In conclusion, Heat and Moisture Exchangers (HMEs) are valuable tools in respiratory care, providing a simple, low-cost method for humidifying and heating the air in mechanically ventilated patients. While they are highly effective for short-term or low-ventilation needs, they have limitations in long-term or high-minute ventilation scenarios. For patients requiring prolonged ventilation, heated humidifiers may offer better humidification and temperature control.
References
- van Oostdam JC, Walker DC, Knudson K, Dirks P, Dahlby RW, Hogg JC. Effect of breathing dry air on structure and function of airways. Journal of Applied Physiology. 1986;61(1):312–317. doi: 10.1152/jappl.1986.61.1.312.
- Fonkalsrud EW, Sanchez M, Higashijima I, Arima E. A comparative study of the effects of dry vs. humidified ventilation on canine lungs. Surgery. 1975;78(3):373–380.
- Mercke U. The influence of varying air humidity on mucociliary activity. Acta Oto-Laryngologica. 1975;79(1-2):133–139. doi: 10.3109/00016487509124665.
- Ballard ST, Inglis SK. Liquid secretion properties of airway submucosal glands. Journal of Physiology. 2004;556(1):1–10. doi: 10.1113/jphysiol.2003.052779.
- Bryant LR. A technique for adequate humidification with mechanical respirators. The Journal of Thoracic and Cardiovascular Surgery. 1963;46:404–407.
- Chatburn RL, Primiano FP., Jr. A rational basis for humidity therapy. Respiratory Care. 1987;32(4):249–254.
- American Association for Respiratory Care, Restrepo RD, Walsh BK. Humidification during invasive and noninvasive mechanical ventilation: 2012. Respiratory Care. 2012;57(5):782–788. doi: 10.4187/respcare.01766.
- Cairo JM. Mosby’s Respiratory Care Equipment. 9th edition. St. Louis, Mo, USA: Mosby, Elsevier; 2013.
- Branson RD. Humidification for patients with artificial airways. Respiratory Care. 1999;44(6):630–641.
- Kacmarek RM, Stoller JK, Heuer AH. Egan’s Fundamentals of Rrespiratory Care. 10th edition.
- Carter BG, Whittington N, Hochmann M, Osborne A. The effect of inlet gas temperatures on heated humidifier performance. Journal of Aerosol Medicine. 2002;15(1):7–13. doi: 10.1089/08942680252908539.
- Nishida T, Nishimura M, Fujino Y, Mashimo T. Performance of heated humidifiers with a heated wire according to ventilatory settings. Journal of Aerosol Medicine: Deposition, Clearance, and Effects in the Lung. 2001;14(1):43–51. doi: 10.1089/08942680152007882.
- Solomita M, Daroowalla F, LeBlanc DS, Smaldone GC. Y-piece temperature and humidification during mechanical ventilation. Respiratory Care. 2009;54(4):480–486.
- Solomita M, Palmer LB, Daroowalla F, et al. Humidification and secretion volume in mechanically ventilated patients. Respiratory Care. 2009;54(10):1329–1335.
- Boots RJ, George N, Faoagali JL, Druery J, Dean K, Heller RF. Double-heater-wire circuits and heat-and-moisture exchangers and the risk of ventilator-associated pneumonia. Critical Care Medicine. 2006;34(3):687–693. doi: 10.1097/01.CCM.0000201887.51076.31.
- Lellouche F, Lyazidi A, Rodriguez P, Brochard L. Condensation in inspiratory and expiratory circuits of heated wire humidifiers, evaluation of a new expiratory, “porous”, circuit and of new humidification compensation systems. Proceedings of the 100th International Conference of the American Thoracic Society; 2005; San Diego, Calif, USA.
- Gilmour IJ, Boyle MJ, Streifel A, McComb RC. The effects of circuit and humidifier type on contamination potential during mechanical ventilation: a laboratory study. The American Journal of Infection Control. 1995;23(2):65–72. doi: 10.1016/0196-6553(95)90096-9.
- http://www.cdc.gov/hicpac/pdf/guidelines/HApneu2003guidelines.pdf.
- Wong DHW. Melted delivery hose—a complication of a heated humidifier. Canadian Journal of Anaesthesia. 1988;35(2):183–186. doi: 10.1007/BF03010661.
- Schumann S, Stahl CA, Möller K, Priebe H-J, Guttmann J. Moisturizing and mechanical characteristics of a new counter-flow type heated humidifier. British Journal of Anaesthesia. 2007;98(4):531–538. doi: 10.1093/bja/aem006.
- Jones SW, Short KA, Joseph M, Sommer C, Cairns BA. Use of a new novel humidification system with high frequency percussive ventilation in a patient with inhalation injury. Journal of Burn Care and Research. 2010;31(3):499–502. doi: 10.1097/BCR.0b013e3181db51e5.
- Hingorani BK. The resistance to airflow of tracheostomy tubes, connections, and heat and moisture exchangers. British Journal of Anaesthesia. 1965;37(6):454–463. doi: 10.1093/bja/37.6.454.
- Vandenbroucke-Grauls CM, Teeuw KB, Ballemans K, Lavooij C, Cornelisse PB, Verhoef J. Bacterial and viral removal efficiency, heat and moisture exchange properties of four filtration devices. Journal of Hospital Infection. 1995;29(1):45–56. doi: 10.1016/0195-6701(95)90292-9.
- Lellouche F, Taillé S, Lefrançois F, et al. Humidification performance of 48 passive airway humidifiers: comparison with manufacturer data. Chest. 2009;135(2):276–286. doi: 10.1378/chest.08-0679.
- Martin C, Perrin G, Gevaudan MJ, Saux P, Gouin F. Heat and moisture exchangers and vaporizing humidifiers in the intensive care unit. Chest. 1990;97(1):144–149. doi: 10.1378/chest.97.1.144.

Add a Comment