High-flow oxygen therapy is a modern method of providing oxygen, through nasal cannulas, with a higher volume of heated and humidified air. This special kind of therapy is also known as high-flow nasal cannula (HFNC). It seems to be a promising alternative therapy because it is less complicated and easier.
The Importance and Measurement of Tidal Volume in Mechanical Ventilation
High-flow oxygen therapy is a modern method of providing oxygen, through nasal cannulas, with a higher volume of heated and humidified air. This special kind of therapy is also known as high-flow nasal cannula (HFNC). It seems to be a promising alternative therapy because it is less complicated and easier.
High Flow Oxygen Therapy: How Long Can It Be Administered?
High-flow oxygen therapy is a modern method of providing oxygen, through nasal cannulas, with a higher volume of heated and humidified air. This special kind of therapy is also known as high-flow nasal cannula (HFNC). It seems to be a promising alternative therapy because it is less complicated and easier.
The Most Common Modes of Mechanical Ventilation
Mechanical ventilation is the process of using an external device (machine) to aid gaseous movement in and out of the lung. It serves as a type of life-saving device that facilitates breathing. Also, it’s widely used as an artificial breathing support in surgical cases, extremely ill situations, or when an individual is incapable of breathing on their own. Various modes of mechanical ventilation play a great role in respiratory support, patient stabilization, and provision of pressure to prevent the alveoli from collapsing. Continue reading, as this article provides you with diverse mechanical ventilation modes and some of the most common modes of air circulation.

Pressure Controlled Ventilation (PCV)
Pressure-controlled ventilation is a special kind of assisted respiration whereby a patient’s inspiratory pressure is predetermined. This mechanical ventilation mode provides an amount of aeration that depends on the compliance of the lungs and the resistance of the alveoli. It is an airflow system where the maximum airway force is constant and the total ventilation fluctuates.
PCV is one of the most convincing pressure-limited ventilation (PLV) that is used regularly in the initial stages of newborn care. It is a technique recommended by different centers for preventing lobar emphysema. Although PCV reduces the risk of barotrauma, it could be challenging to provide a sufficient tidal volume (VT) when used in patients with ARDS. Also, an improper setting of this ventilator can lead to hypoxia and respiratory depression.

Volume Controlled Ventilation (VCV)
The modes of mechanical ventilation that involves a preset tidal volume to be provided in a specific amount of time is volume-controlled ventilation. It is usually more simple and comprehensible for most medical practitioners new to assisted air circulation. In this case, total ventilation is always set, the volume of breath supplied is constant, but the inspiratory pressure is unstable.
Most of the time, VCV is commonly used in anesthesia, either in the assisted control (AC) mode or continuous mandatory ventilation (CMV). Due to the increase in peak pressure (PIP) with steady and accurate breathing volume, it usually causes uneven gaseous distribution and volutrauma.
Pressure Support Ventilation (PSV)
A special mode of positive-pressure mechanical ventilation that requires patient initiation of each breath is known as pressure support ventilation. This kind of aided respiration can be administered either through the use of intubation (invasive) or with a mask (non-invasive) ventilatory pattern. It’s known as the most pleasant aided airflow with a useful system that delivers the benefits of the two types of ventilator patterns.
PSV involves setting maximum driving pressure which usually indicates the ventilator flow rate. Sometimes, the patient’s pulmonary compliance, airway resistance, PIP, and breathing efforts frequently affect this flow rate. There is no minimum minute ventilation and the tidal volume provided is influenced by the flow and rate of breathing. Due to a volatile VT, it may also make the lung distend excessively.
Pressure-Limited Time-Cycled Ventilation
Another type of PLV (similar to a pressure-controlled ventilator) that was previously used in neonates is the time-cycled PLV. This mechanical ventilation mode makes use of a predetermined peak pressure and a specified volume of gas within an extended period. While breathing in, this triggered ventilator provides a steady flow of air to the patient.
Previous reports about the use of pressure-limited time-cycled ventilation have shown that lungs are usually susceptible to atelectrauma and barotrauma conditions. In addition, it has been observed that one of the primary factors influencing ventilator-associated lung injury (VALI) is Total ventilation (VT).

Synchronized Intermittent Mandatory Ventilation (SIMV)
This is a unique mode of mechanical ventilation that provides a fixed tidal volume at a predefined frequency. In most cases, synchronized intermittent mandatory air circulation always permits patients to voluntarily breathe on their own. SIMV produces a mandatory breath that is delivered at the same moment the patient starts initiating their breath (spontaneous breath). In addition, positive end-expository pressure (PEEP) can also be administered using this synchronized IMV method.
SIMV is mostly required by people with COPD, neuromuscular disorder, or ARDS and is used alongside pressure support ventilation. In some instances where SIMV is improperly used, there may be an inability to initiate spontaneous breath, fluctuations in intrathoracic force, or severe respiratory failure. This technique of ventilation is risky for hyperventilation, consumes much time, and can cause infection, barotrauma, or cardiac arrhythmias.

High Flow Nasal Cannula (HFNC)
A high-flow nasal cannula is an oxygen therapy commonly called a heated, humidified, high-flow nasal cannula (HHFNC). It entails the delivery of a flexible blend of warmed, humid, and oxygen-rich air at a variable pace that surpasses spontaneous pulmonary flow. Whenever this aeration is used to provide oxygen, the flow is significantly greater than that with conventional nasal cannulas.
In addition, HFNC enhances the functional residual capacity, and accurate distribution of oxygen. This mechanical ventilation mode often has an outcome of improved breathing efficiency due to continuous high oxygen flow that often washes out the anatomical dead space.
Self Adjustable Ventilation (SAV)
Self Adjustable Ventilation is a special ventilator that makes use of detectors to constantly alter the airflow in response to changes in air properties. With the help of this technique, indoor comfort, improved air exchange systems, and environmental sustainability are guaranteed. This often allows great flexibility in ventilator parameters and also blends soothingly with a wide range of conditions.
References
1.https://my.clevelandclinic.org/health/treatments/15368-mechanical-ventilation
2.https://www.sciencedirect.com/topics/medicine-and-dentistry/pressure-controlled-ventilation
3. https://ecampusontario.pressbooks.pub/mechanicalventilators/chapter/volume-control-ventilation/
4.https://ecampusontario.pressbooks.pub/mechanicalventilators/chapter/volume-control-ventilation/
5.https://pubmed.ncbi.nlm.nih.gov/31536312/#:~:text=
7. https://www.icliniq.com/articles/respiratory-health/synchronized-intermittent-mandatory-ventilation
8.https://www.uptodate.com/contents/high-flow-nasal-cannula-oxygen-therapy-in-children
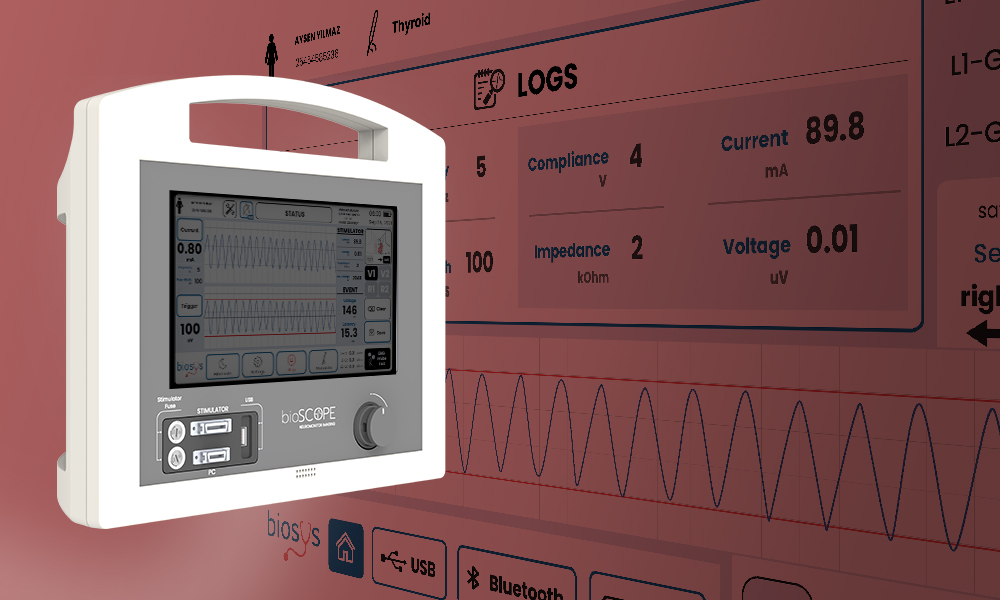
NEWS – Turkish factory Biosys exports respiratory devices to 41 countries
In Batman Organize Sanayi Bolgesi (OSB), respiratory devices manufactured in a factory are exported to 41 countries.
During the COVID-19 pandemic, Biosys, a domestic producer of respiratory devices, collaborated with Arcelik, ASELSAN, and Baykar under the guidance of the Ministry of Health and the Ministry of Industry and Technology.
Both, in collaboration, inaugurated a factory in Batman OSB on March 6 of this year, with the presence of the Minister of Treasury and Finance Mehmet Simsek and Mehmet the Minister of Industry and Technology Fatih Kacir.
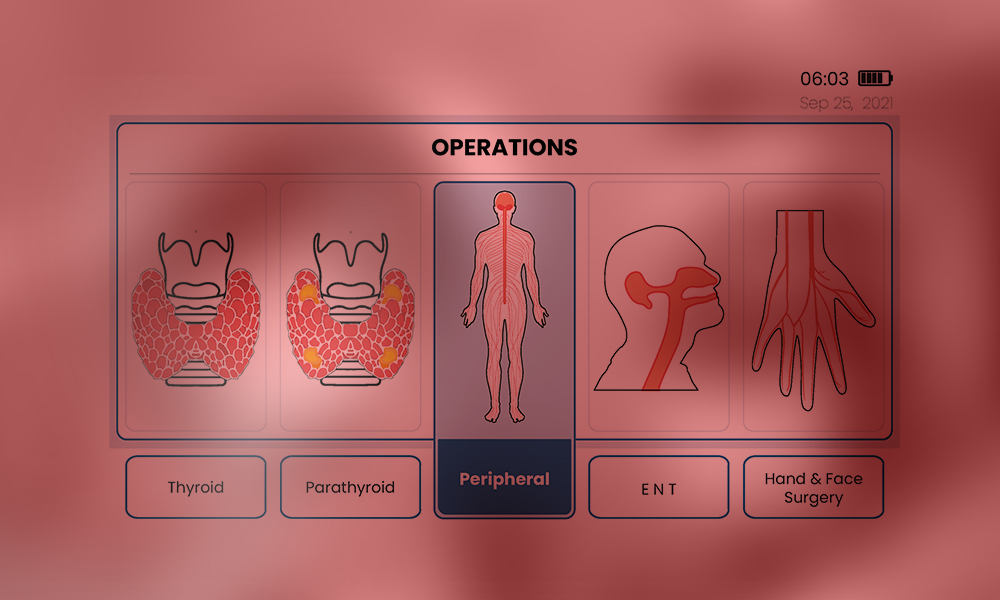
Advantages of Using Neuromonitoring in Surgical Operations
Explore the technological advancement in mechanical ventilators as this article will provide you with a historical knowledge of ventilators, some of the modern innovations in ventilator technology, and the future of ventilation.
The Evolution of ICU Ventilators: Past, Present, and Future
Explore the technological advancement in mechanical ventilators as this article will provide you with a historical knowledge of ventilators, some of the modern innovations in ventilator technology, and the future of ventilation.
Understanding Neuromonitoring: Applications and Advancement
During an operation, surgeons often employ various activities such as intraoperative monitoring (IOM) to achieve the ideal goal of saving lives. However, in cases related to the nervous system an IOM subdivision process called Neuromonitoring or Electrophysiologic monitoring is often employed.
It provides a monitoring purpose that notifies the anesthesia specialist and operating neurologist of an approaching injury so that they can adjust the course of treatment in time to avoid irreversible harm.
This is sometimes used to create and locate neuron regions to help provide technical management. It is a strategy that is employed to reduce possible risks associated with the neural network.
Continue reading as this article provides you with information about the meaning of intraoperative neuromonitoring (IONM), its basics, clinical application, and its technical future directions.
What’s Intraoperative Neuromonitoring?
One of the medical procedures that entails constant checks of brain and neuronal activities during neural operations is known as intraoperative neuromonitoring (IONM). This procedure aids in the structural presentation of the sensorium and also illustrates its likely associated impairments.
Its main objective is to maintain the neurological system’s ideal nature, most especially the central nervous system (CNS) and the peripheral nerve. In addition, IONM provides neurophysiological data, which presents safer and more comprehensive processes that can be executed by the neurologist.
Basics of Neuromonitoring: What you need to know?
In many medical procedures, neuromonitoring has become the standard and has taken the place of intraoperative wake-up testing in spinal surgery. However, there are no evaluating terms and standards of care as most monitoring teams and surgeons choose their methods. Below are its basics:
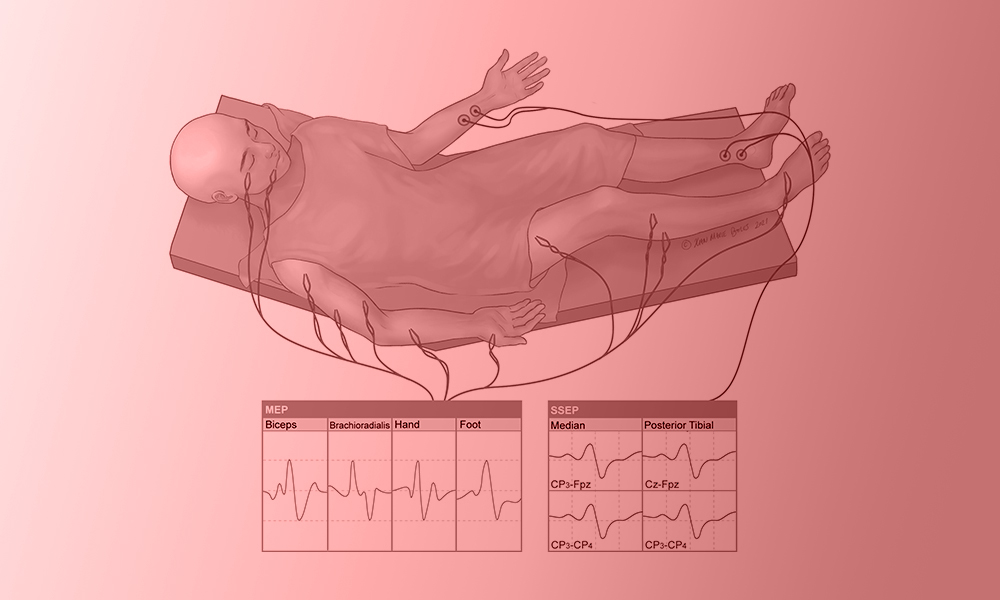
- Objective: During an operation, neuromonitoring is often used to obtain nerves’ electrical potentials produced by their axons. This is carried out to prevent and identify problems before escalating and to reduce any possible complications.
- Methods: there are various methods used for surgical neuromonitoring. These are:
- Electromyography (EMG): is used for recording muscular activities.
- Electroencephalography (EEG): is utilized for measuring brain activity.
- Motor Evoked Potential (MEP): This is often used for evaluating motor pathway function.
- Somatosensory Evoked Potentials (SSEP): To track sensory pathways integrity.
- Application: Neuromonitoring in surgery is often applied in different ways to a wide range of neurological problems eg. Cranial neurosurgery, interventional radiological procedures, Orthopedic spinal correction, stroke, hypoxic-ischemic injury, meningitis, etc.
- Procedure: To measure brain reactions, perfectly placed electrodes are applied to the patient, and baseline values are recorded before the commencement of the surgical operation. Throughout the process, there is always proper evaluation, and a swift reaction is often taken whenever there is a baseline alteration.
- Teamwork: There is always a cordial interaction between Neurologists, surgeons, and anesthetic teams to obtain current data about brain activity. With this obtained data, the surgical team needs to discuss possible steps and plans among themselves that will help in direct clinical decision-making.
- Continuous Evaluation: As the operation continues, there is always a concurrent check that makes the surgeons quickly identify any possible variation in nerve function to make any necessary corrections.
Cutting-Edge Applications in Neuromonitoring Clinical Settings
With the rapid changes and developments in today’s neuromonitoring technology, significant advances have been made in the medical world. These modern techniques in clinical settings have improved immediate nervous system diagnosis and protection. Here are some conspicuous examples:
- Advanced Intraoperative MRI: During surgeries, an intraoperative radiological imaging device provides structural or regional images that aid quick nervous detection by neurologists. These magnetic resonated images facilitate easy access to various modifications in the brain or spinal cord.
- Optical Coherence Tomography (OCT): The images of some complex optical regions like the optic nerve, and retina can be obtained at high quality. It has been put to use many times to diagnose and manage diabetes’s effect on the retina in conditions like glaucoma and retinopathy.
- High-Resonance Image: The application of neuromonitoring in surgeries provides an exceptional method for surgeons to craft comprehensive preoperative planning. Most of the time, it grants fast access to complications during operations with its additional high-resonating imaging features.
- Neural stimulation Technique: It comprises advanced methods that use magnetic or electrical stimulation to modify the neuronal response. Also, this technique is often used to map and protect important brain circuits.
- Mechanical Alarming System: This is one of the most important innovative applications of surgical neuromonitoring that improves responsiveness. This system automatically identifies and notifies surgical teams of possible problems with the help of AI algorithms.
Clinical Application of Neuromonitoring in Surgery
The application of surgical neuromonitoring methods involves a wide range of healthcare processes that improve patients’ outcomes. Some of its vital applications in medics are:
- Surgeries on the brain: Neuromonitoring helps evaluate and protect vital cranial functions during brain surgeries, reducing the possibility of neurological implications. It is used during brain tumor removal and epileptic surgery.
- Spinal Cord Surgery: Intraoperative neuromonitoring plays an exceptional role in countless surgeries related to the spine. Some of these are laminectomy, spinal decompression, and fusion. IONM also acts as a protective medium for the spine to evaluate nerve fibers during surgeries.
- Musculoskeletal surgery: In conditions related to the skeletal system (joint, suture, or skull) the use of neuromonitoring in surgery is of great significance. Some orthopedic surgeries like laminectomy and kyphoplasty are special operations where electrophysiology monitoring methods can be employed.
- Complicated Pediatric Operations: The nervous system in children with complicated medical conditions such as scoliosis and spinal tumors, is monitored to avoid neuronal growth retardation.
- Otolaryngological Operations: Intraoperative neuromonitoring helps maintain important neural structures during head and neck surgeries, such as the removal of an auditory neuroma or treatments involving the seventh cranial nerve.
Future Directions in Neuromonitoring Technology
In recent years, there have been countless growth and advancements in the use of surgical neuromonitoring technology. However, It is believed that technically neuromonitoring in surgery will progress in several important areas in the future. Such as:
- AI Integration: Neuromonitoring devices may improve immediate data processing by using AI algorithms. This might lead to quicker and more accurate neurological signal clarifications, which would help surgeons make instant critical decisions.
- Multifunctional Technique: A more enhanced view can be achieved via the combination of different IONM methods. A technique that encompasses an all-in-one (coupling of EMG, EEG, MEP, and SSEP) neuromonitoring in surgery will serve a great function for surgeons.
- Digital Assessment and Telesurgery: A more technologically developed neuromonitoring can create a telesurgical approach whereby non-physical surgeons will have the opportunity to operate.
- Mobile Access: In the future, the use of wireless surgical neuromonitoring devices can be invented creating an effective medium for tracking the medical progress of a patient. This can also result in easy integration of surgical equipment, enhancing a more versatile operative room.
Neuromonitoring technological advancements have transformed surgical procedures in clinical settings by providing immediate evaluation and nervous system protection. By improving patient outcomes, these advancements mark the beginning of an inventive age in neurosurgery and spine therapies.
You can explore this evolving field of intraoperative neuromonitoring methods and discover modern applications and technological developments that guarantee safer surgical procedures. Dive into the future with the advancement of surgical neuromonitoring that comes along with a lot of factors that improves patient outcomes.
References
- https://www.sciencedirect.com/topics/medicine-and-dentistry/intraoperative-monitoring
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8526228/
- https://www.hopkinsmedicine.org/neurology-neurosurgery/specialty-areas/ionm
- https://www.kines.umich.edu/academics/movement-science/undergraduate/intraoperativeneuromonitoringionm-program
- https://www.longdom.org/open-access/neuromonitoring-in-anesthesia-current-practices-and-future-directions-104519.html#:~:
How Do Patient Outcomes Improve With Advanced Humidification In Ventilation?
One of the major systems in the human body that is responsible for the control of gaseous exchange is the respiratory system. Sometimes, this breathing pathway may be damaged due to certain conditions resulting in improper ventilation mechanisms. However, with the invention of humidifier ventilation, most of these respiratory inconveniences and difficulties can be avoided.
Initially, the human airway performs the function of an additional provision of water vapor (moisture) to inspire air which enhances pulmonary activities. This process of additional moisture known as a humidification mechanism is often provided by what is called a ventilator humidifier in a mechanical ventilator.
However, there have been a series of improvements in clinical technology providing an adequate medical system that maximizes patient outcomes. This article will provide you with comprehensive details about humidification, its key roles, strategic implementation, and success stories in ICU settings.
What’s Respiratory Humidification?
The process of adding moisture, heat, and filtrating inhaled air in mechanical ventilators to aid convenient breathing similar to normal is known as Respiratory humidification. It is an integral process that provides lung protection, comfortable respiration, and above all keeps the airway safe.
The Role of Humidification in Respiratory Care
Generally speaking, patients in the ICU setting often benefit from the great impact of humidification, as it provides them with so much improved respiratory care. Some Integral roles performed by humidification are:
- Upper Airway protection: The addition of saturated water molecules makes inspired air filled with moisture that helps in the protection of the mucosa lining the nostrils and pharynx (airway).
- Enhance Gaseous Exchange: With the help of ventilator humidifiers, proper diffusion, and exchange of inspired air are carried out within the lungs and with the environment.
- Patient Comfort: One of the most integral roles of humidifier ventilation is in its comforting mechanism aided by providing fresh breath without tampering with the airway or causing havoc to the lungs. In addition to this comfort, it provides perfect tolerance and compliance.
- Regulate Temperature: The humidification process provides a regulated inspired air preventing the cause of any thermal-related problems e.g. hypothermia. It helps in the regulation of the internal body temperature which aids in proper medical treatment.
- Prevent Complications: The presence of a ventilator humidifier prevents patients from developing various respiratory problems or damages. It protects them from conditions like bronchospasm, infections, mucous plugging, and lots more due to the humid passage through the lungs.
- Decrease Airway Resistance: Ventilation humidifier also plays a significant role in preserving the airway’s natural humidity balance and also reduces airway resistance.
- Long-term Ventilation Assistance: In most cases that require prolonged respiratory care, an advanced positive pressure mechanism, incorporated with humidifier ventilation is often utilized to preserve the system and solve the difficulties.

Case Studies: Success Stories in ICU Settings
The use of humidifier ventilators in ICU settings has brought great advancement in the healthcare sector by producing increased success stories and patient outcomes. Below are some ventilator’s impact success stories.
Case Study 1: The Impact of Humidifier Ventilation in John’s COPD Maintenance
A forty-year-old man, called John, experiences a miraculous treatment that helps preserve his severe breathing condition. His amazing recovery was achieved due to the impact of humidifier ventilation during his brief stay in the ICU setting.
He is a refinery worker with a medical background of 3 years of COPD. He was brought to the healthcare center with various likely symptoms like persistent wheezing, shortness of breath, and chest pain after a long morning exercise he had that morning.
After a proper diagnosis, a bullectomy surgery was considered a perfect solution by the medical team to preserve John’s life. A strategic plan was structured by the medical team to perform the surgery.
The surgery was a success following the perfect removal of giant bullae (air pockets) in the left lung. After the surgical procedure, the concurrent chest pain was reduced, and was entirely placed on the non-invasive humidifier ventilator.
John’s surgery was a success, and he was referred to the ICU setting as he was permanently placed on a positive pressure ventilation system coupled with a ventilator humidifier.
In conclusion, the humidifier ventilation method was administered to enhance his respiratory function. He was discharged and further assisted via telemedicine care.

Case Study 2: Angela’s tale of recovery from Acute Asthma with a Ventilator Humidifier in ICU
Angela, a young girl, was brought into an accident and emergency unit. For the sake of saving her life, an asthmatic-relieving drug was administered and then placed on a non-invasive ventilator humidifier.
Her medical symptoms and background show that she is having difficulty breathing, wheezing, and shortness of breath, and has been managing the condition since 8 years old.
Quickly, she was first stabilized and referred to the ICU, where she was placed on an NIV ventilator humidifier. She was constantly monitored throughout the process.
She was assigned some medical specialists, like respiratory therapists and pediatricians, who work tirelessly to achieve their medical goals.
Due to her age, she was carefully monitored and assisted by several nurses. After about three to five days in the intensive care unit, her respiratory system was observed to improve, and she was also breathing perfectly well. She was discharged from the ICU setting in good condition.
Best Practice for Implementing Humidification
The use of a ventilator humidifier requires some procedures for the enhancement of general healthcare. To implement humidification, the following procedures are to be practiced:
- Determine Perfect Humidification Method: The selection of a perfect humidification method, either an active-passive humidifier or a heated humidifier, is vital for medical well-being.
- Monitor Temperature and Humidity: Constant checks should be taken on the appropriate level of humidity and temperature. This helps lessen inflammation and airway dryness and should be maintained according to patient demand.
- Sterile Water Utilization: Sterile Water is the best that can be used for airway humidification that won’t expose the patient to pollution or external factors.
- Routine Cleaning and Maintenance: To avoid microbial development and preserve ventilator maximum efficiency, rigorous adherence to proper upkeep and cleaning systems must be executed for various humidification components.
- Use of Heat and Moisture Exchanger Filters: These filters are a good component that helps to preserve humidity and also reduce infection tendency. The proper use of this filter will grant the body defense to external bodies.
- Sensor Check: When checking the degree of humidity consistently, the humidifier ventilator may automatically change settings with the help of an in-built sensor.
You can be a partaker of a respiratory system like no other with the aid of an advanced humidification system. This alternative breathing method is a type that brings more comfort, satisfaction and improved pulmonary treatment. However, you can also be a participant in this transformative respiratory care by taking a step today with a humidified ventilation system.
References
Advancement in Non-Invasive Ventilation
Dated to the 1940s, Non-invasive Ventilation has been undergoing a series of changes with various modifications in designs and techniques. This improvement in ventilator modes has exceeded imaginations and has brought a lot of technical healthcare solutions to diverse medical problems.
Evolution of Non-Invasive Ventilation Technology
NIV as a mode of ventilation has a great impact in the intensive care unit, as it provides a life-changing option that produces more positive outcomes. In addition, its impact on humanity is much more than an invention but one with immeasurable support and medical advancement that comes with a decrease in problems associated with intubation.
This article shall discuss some of the clinical importance of non-invasive ventilation in comparison with the invasive method, its impact on patient outcomes, its various technical and clinical benefits, alongside some of the future trends NIV possesses.

What’s Non-Invasive Ventilation?
One of the special modes of ventilation that does not require the use of a penetrating apparatus (endotracheal intubation) to aid respiration is known as Non-invasive ventilation (NIV). This is a unique method that is often employed to reduce complications associated with invasive ventilation eg. acute respiratory failure, airway disorder, etc. It is a technique with various forms of suitable designs and modifications that help in maintaining chronic respiratory conditions.
What Are The Clinical Benefits And Patient Outcomes of Positive Pressure Ventilation (NIV)?
Assisted ventilation in humans comes in various ways, one of which is the process of using positive pressure to aerate the lungs. This mode of ventilation is often called Positive pressure ventilation. In most cases, this method is always utilized in a non-invasive ventilation system with diverse advantages and benefits compared to others.

Medical Benefits and Technological Advancement of Non-invasive Ventilation
- Special Treatment Provision: Non-invasive ventilation in the healthcare system serves as a special equipment that is used for the treatment of diverse chronic and mild conditions. Oftentimes, this positive pressure ventilation device in the BiPAP method serves as a standard unique treatment method recommended for some specific respiratory failure and occasional health safety (OHS) e.g. AHRF, pneumonia, etc.
- Used for Obstructive sleep apnea: Due to NIVs’ evolving features (i.e. a developed user interface), it is often utilized in many chronic and acute respiratory cases such as the treatment of obstructive sleeping apnea (OSA). This evolution has produced facial and nasal means of breathing pressure (CPAP) aimed at treating sleep-related respiratory disorders.
- Chronic Respiratory Management: Currently, NIV is a ventilator mode used as a proven treatment for patients with COPD problems and related chronic respiratory problems like neuromuscular abnormalities.

Technological Advancement of NIV Ventilator Mode
- Advanced Human Interface: More effective mask designs that have stronger sealing qualities, and air-leakage reduction which improve patient comfort are some NIV distinct attributes. These features mostly allow usage by a wide range of patient demography (young babies, adults, pregnant women, etc.)
- Automated Monitoring System: With the help of a modern detector and monitoring system, it ensures an accurate pressure setting. This integrated detector also supplies real-time data collections that assist medical professionals to track patients’ progress and modify treatment plans.
- Telehealth Implementation: Some technical advancements in NIV ventilator mode such as telehealth integration have been an advantage for most healthcare providers to monitor their patient health status remotely.
Non-Invasive Ventilation Patient’s Outcome
The impact of non-invasive ventilation on life has gained remarkable attention and patients with a range of breathing complications have been greatly helped and their health alongside their quality of life have improved. Below are some patient outcomes of non-invasive ventilation:
- Enhanced Respirational Ability: Oftentimes, patients with respiratory complications after being placed on NIV positive pressure ventilation, usually have an improved ability to respire. Appropriate amounts of oxygen have been obtained and various breathing complications are lessened.
- Reduction in Death Rate: According to studies, the impact of these modes of ventilation on life has caused a considerable reduction in mortality rate. Most cases like COPD can be managed leading to auspicious survival results: an effect orchestrated by non-invasive ventilation initiation.
- Decreased Rates of Intubation: The use of positive pressure ventilation can help avoid or reduce the requirement for invasive ventilation mechanisms. Patients who avoid intubation face fewer of the risks that come with invasive procedures.
- Improved Comfort and Adherence of Patients: Non-invasive ventilation (NIV) offers a higher degree of patient comfort. It Improves patient compliance with recommended therapies and serves as a direct result of increased comfort, which guarantees long-term therapy advantages.
Clinical Advantages of NIV over Invasive Ventilation
Clinically and technically, Non-invasive ventilation has an edge over invasive ventilation. It possesses a lot of features that are of great remark. The advantages of non-invasive ventilation are beyond measures in the medical application and we have some as follows:
- Reduce cost: When considering extended hospital stays and the requirement for critical care services, NIV is frequently linked to decreased healthcare expenditures compared to invasive ventilation.
- Decreased Infection Risk: By doing away with intrusive procedures like intubation, Non-invasive ventilation lowers the risk of pneumonia and other ventilator-associated illnesses.
- Reduction in Barotrauma Risk: The risk of barotrauma, in which high pressure damages the lungs, exists with invasive respiration. However, diminished pressure settings in NIV lessen this danger and diminish the possibility of lung damage brought on by the ventilator.
- Promotes Oral Health and Communication: Compared to patients with endotracheal tubes, patients under NIV have greater ease of communication, eating, and oral hygiene, which improves patient wellness and overall quality of life.
- Use at home is possible: You can use the NIV mode of ventilation with no need for airway skills. Its usage requires less medical prowess compared to invasive ventilation.
Future Trends in Non-Invasive Respiratory Support
In the medical field, there are a series of expected developments in technological modifications of clinical equipment. One of these devices that has been a major concern is the non-invasive ventilator (NIV). This appliance has been an incredible device linked with improving patient outcomes with its possible future trends. These future trends are said to optimize ventilation settings and improve personalized healthcare, with the integration of exceptional features such as:
- Algorithm and Artificial Intelligence
- Portable Design
- Wearable device format
- Improved Telehealth System
- Biocompatible
- Enhanced User interface etc.
References
- https://pubmed.ncbi.nlm.nih.gov/19111105/
- https://rc.rcjournal.com/content/64/6/712
- https://breathe.ersjournals.com/content/9/5/338
- https://www.physio-pedia.com/Non_Invasive_Ventilation
- https://onlinelibrary.wiley.com/doi/full/10.1111/resp.13497
- https://www.ncbi.nlm.nih.gov/books/NBK578188/
- https://bmcpulmmed.biomedcentral.com/articles/10.1186/s12890-016-0289-y
- https://breathe.ersjournals.com/content/13/2/84