Explore the technological advancement in mechanical ventilators as this article will provide you with a historical knowledge of ventilators, some of the modern innovations in ventilator technology, and the future of ventilation.
Understanding Neuromonitoring: Applications and Advancement
During an operation, surgeons often employ various activities such as intraoperative monitoring (IOM) to achieve the ideal goal of saving lives. However, in cases related to the nervous system an IOM subdivision process called Neuromonitoring or Electrophysiologic monitoring is often employed.
It provides a monitoring purpose that notifies the anesthesia specialist and operating neurologist of an approaching injury so that they can adjust the course of treatment in time to avoid irreversible harm.
This is sometimes used to create and locate neuron regions to help provide technical management. It is a strategy that is employed to reduce possible risks associated with the neural network.
Continue reading as this article provides you with information about the meaning of intraoperative neuromonitoring (IONM), its basics, clinical application, and its technical future directions.
What’s Intraoperative Neuromonitoring?
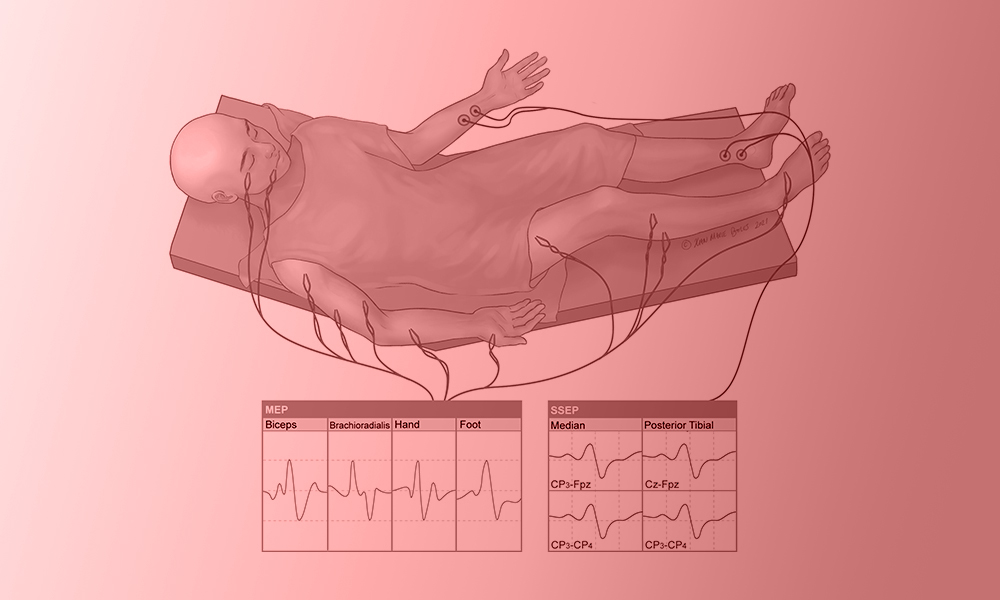
One of the medical procedures that entails constant checks of brain and neuronal activities during neural operations is known as intraoperative neuromonitoring (IONM). This procedure aids in the structural presentation of the sensorium and also illustrates its likely associated impairments.
Its main objective is to maintain the neurological system’s ideal nature, most especially the central nervous system (CNS) and the peripheral nerve. In addition, IONM provides neurophysiological data, which presents safer and more comprehensive processes that can be executed by the neurologist.
Basics of Neuromonitoring: What you need to know?
In many medical procedures, neuromonitoring has become the standard and has taken the place of intraoperative wake-up testing in spinal surgery. However, there are no evaluating terms and standards of care as most monitoring teams and surgeons choose their methods. Below are its basics:
- Objective: During an operation, neuromonitoring is often used to obtain nerves’ electrical potentials produced by their axons. This is carried out to prevent and identify problems before escalating and to reduce any possible complications.
- Methods: there are various methods used for surgical neuromonitoring. These are:
- Electromyography (EMG): is used for recording muscular activities.
- Electroencephalography (EEG): is utilized for measuring brain activity.
- Motor Evoked Potential (MEP): This is often used for evaluating motor pathway function.
- Somatosensory Evoked Potentials (SSEP): To track sensory pathways integrity.
- Application: Neuromonitoring in surgery is often applied in different ways to a wide range of neurological problems eg. Cranial neurosurgery, interventional radiological procedures, Orthopedic spinal correction, stroke, hypoxic-ischemic injury, meningitis, etc.
- Procedure: To measure brain reactions, perfectly placed electrodes are applied to the patient, and baseline values are recorded before the commencement of the surgical operation. Throughout the process, there is always proper evaluation, and a swift reaction is often taken whenever there is a baseline alteration.
- Teamwork: There is always a cordial interaction between Neurologists, surgeons, and anesthetic teams to obtain current data about brain activity. With this obtained data, the surgical team needs to discuss possible steps and plans among themselves that will help in direct clinical decision-making.
- Continuous Evaluation: As the operation continues, there is always a concurrent check that makes the surgeons quickly identify any possible variation in nerve function to make any necessary corrections.
Cutting-Edge Applications in Neuromonitoring Clinical Settings
With the rapid changes and developments in today’s neuromonitoring technology, significant advances have been made in the medical world. These modern techniques in clinical settings have improved immediate nervous system diagnosis and protection. Here are some conspicuous examples:
- Advanced Intraoperative MRI: During surgeries, an intraoperative radiological imaging device provides structural or regional images that aid quick nervous detection by neurologists. These magnetic resonated images facilitate easy access to various modifications in the brain or spinal cord.
- Optical Coherence Tomography (OCT): The images of some complex optical regions like the optic nerve, and retina can be obtained at high quality. It has been put to use many times to diagnose and manage diabetes’s effect on the retina in conditions like glaucoma and retinopathy.
- High-Resonance Image: The application of neuromonitoring in surgeries provides an exceptional method for surgeons to craft comprehensive preoperative planning. Most of the time, it grants fast access to complications during operations with its additional high-resonating imaging features.
- Neural stimulation Technique: It comprises advanced methods that use magnetic or electrical stimulation to modify the neuronal response. Also, this technique is often used to map and protect important brain circuits.
- Mechanical Alarming System: This is one of the most important innovative applications of surgical neuromonitoring that improves responsiveness. This system automatically identifies and notifies surgical teams of possible problems with the help of AI algorithms.
Clinical Application of Neuromonitoring in Surgery
The application of surgical neuromonitoring methods involves a wide range of healthcare processes that improve patients’ outcomes. Some of its vital applications in medics are:
- Surgeries on the brain: Neuromonitoring helps evaluate and protect vital cranial functions during brain surgeries, reducing the possibility of neurological implications. It is used during brain tumor removal and epileptic surgery.
- Spinal Cord Surgery: Intraoperative neuromonitoring plays an exceptional role in countless surgeries related to the spine. Some of these are laminectomy, spinal decompression, and fusion. IONM also acts as a protective medium for the spine to evaluate nerve fibers during surgeries.
- Musculoskeletal surgery: In conditions related to the skeletal system (joint, suture, or skull) the use of neuromonitoring in surgery is of great significance. Some orthopedic surgeries like laminectomy and kyphoplasty are special operations where electrophysiology monitoring methods can be employed.
- Complicated Pediatric Operations: The nervous system in children with complicated medical conditions such as scoliosis and spinal tumors, is monitored to avoid neuronal growth retardation.
- Otolaryngological Operations: Intraoperative neuromonitoring helps maintain important neural structures during head and neck surgeries, such as the removal of an auditory neuroma or treatments involving the seventh cranial nerve.
Future Directions in Neuromonitoring Technology
In recent years, there have been countless growth and advancements in the use of surgical neuromonitoring technology. However, It is believed that technically neuromonitoring in surgery will progress in several important areas in the future. Such as:
- AI Integration: Neuromonitoring devices may improve immediate data processing by using AI algorithms. This might lead to quicker and more accurate neurological signal clarifications, which would help surgeons make instant critical decisions.
- Multifunctional Technique: A more enhanced view can be achieved via the combination of different IONM methods. A technique that encompasses an all-in-one (coupling of EMG, EEG, MEP, and SSEP) neuromonitoring in surgery will serve a great function for surgeons.
- Digital Assessment and Telesurgery: A more technologically developed neuromonitoring can create a telesurgical approach whereby non-physical surgeons will have the opportunity to operate.
- Mobile Access: In the future, the use of wireless surgical neuromonitoring devices can be invented creating an effective medium for tracking the medical progress of a patient. This can also result in easy integration of surgical equipment, enhancing a more versatile operative room.
Neuromonitoring technological advancements have transformed surgical procedures in clinical settings by providing immediate evaluation and nervous system protection. By improving patient outcomes, these advancements mark the beginning of an inventive age in neurosurgery and spine therapies.
You can explore this evolving field of intraoperative neuromonitoring methods and discover modern applications and technological developments that guarantee safer surgical procedures. Dive into the future with the advancement of surgical neuromonitoring that comes along with a lot of factors that improves patient outcomes.
References
- https://www.sciencedirect.com/topics/medicine-and-dentistry/intraoperative-monitoring
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8526228/
- https://www.hopkinsmedicine.org/neurology-neurosurgery/specialty-areas/ionm
- https://www.kines.umich.edu/academics/movement-science/undergraduate/intraoperativeneuromonitoringionm-program
- https://www.longdom.org/open-access/neuromonitoring-in-anesthesia-current-practices-and-future-directions-104519.html#:~:
How Do Patient Outcomes Improve With Advanced Humidification In Ventilation?
One of the major systems in the human body that is responsible for the control of gaseous exchange is the respiratory system. Sometimes, this breathing pathway may be damaged due to certain conditions resulting in improper ventilation mechanisms. However, with the invention of humidifier ventilation, most of these respiratory inconveniences and difficulties can be avoided.
Initially, the human airway performs the function of an additional provision of water vapor (moisture) to inspire air which enhances pulmonary activities. This process of additional moisture known as a humidification mechanism is often provided by what is called a ventilator humidifier in a mechanical ventilator.
However, there have been a series of improvements in clinical technology providing an adequate medical system that maximizes patient outcomes. This article will provide you with comprehensive details about humidification, its key roles, strategic implementation, and success stories in ICU settings.

What’s Respiratory Humidification?
The process of adding moisture, heat, and filtrating inhaled air in mechanical ventilators to aid convenient breathing similar to normal is known as Respiratory humidification. It is an integral process that provides lung protection, comfortable respiration, and above all keeps the airway safe.
The Role of Humidification in Respiratory Care
Generally speaking, patients in the ICU setting often benefit from the great impact of humidification, as it provides them with so much improved respiratory care. Some Integral roles performed by humidification are:
- Upper Airway protection: The addition of saturated water molecules makes inspired air filled with moisture that helps in the protection of the mucosa lining the nostrils and pharynx (airway).
- Enhance Gaseous Exchange: With the help of ventilator humidifiers, proper diffusion, and exchange of inspired air are carried out within the lungs and with the environment.
- Patient Comfort: One of the most integral roles of humidifier ventilation is in its comforting mechanism aided by providing fresh breath without tampering with the airway or causing havoc to the lungs. In addition to this comfort, it provides perfect tolerance and compliance.
- Regulate Temperature: The humidification process provides a regulated inspired air preventing the cause of any thermal-related problems e.g. hypothermia. It helps in the regulation of the internal body temperature which aids in proper medical treatment.
- Prevent Complications: The presence of a ventilator humidifier prevents patients from developing various respiratory problems or damages. It protects them from conditions like bronchospasm, infections, mucous plugging, and lots more due to the humid passage through the lungs.
- Decrease Airway Resistance: Ventilation humidifier also plays a significant role in preserving the airway’s natural humidity balance and also reduces airway resistance.
- Long-term Ventilation Assistance: In most cases that require prolonged respiratory care, an advanced positive pressure mechanism, incorporated with humidifier ventilation is often utilized to preserve the system and solve the difficulties.

Case Studies: Success Stories in ICU Settings
The use of humidifier ventilators in ICU settings has brought great advancement in the healthcare sector by producing increased success stories and patient outcomes. Below are some ventilator’s impact success stories.
Case Study 1: The Impact of Humidifier Ventilation in John’s COPD Maintenance
A forty-year-old man, called John, experiences a miraculous treatment that helps preserve his severe breathing condition. His amazing recovery was achieved due to the impact of humidifier ventilation during his brief stay in the ICU setting.
He is a refinery worker with a medical background of 3 years of COPD. He was brought to the healthcare center with various likely symptoms like persistent wheezing, shortness of breath, and chest pain after a long morning exercise he had that morning.
After a proper diagnosis, a bullectomy surgery was considered a perfect solution by the medical team to preserve John’s life. A strategic plan was structured by the medical team to perform the surgery.
The surgery was a success following the perfect removal of giant bullae (air pockets) in the left lung. After the surgical procedure, the concurrent chest pain was reduced, and was entirely placed on the non-invasive humidifier ventilator.
John’s surgery was a success, and he was referred to the ICU setting as he was permanently placed on a positive pressure ventilation system coupled with a ventilator humidifier.
In conclusion, the humidifier ventilation method was administered to enhance his respiratory function. He was discharged and further assisted via telemedicine care.

Case Study 2: Angela’s tale of recovery from Acute Asthma with a Ventilator Humidifier in ICU
Angela, a young girl, was brought into an accident and emergency unit. For the sake of saving her life, an asthmatic-relieving drug was administered and then placed on a non-invasive ventilator humidifier.
Her medical symptoms and background show that she is having difficulty breathing, wheezing, and shortness of breath, and has been managing the condition since 8 years old.
Quickly, she was first stabilized and referred to the ICU, where she was placed on an NIV ventilator humidifier. She was constantly monitored throughout the process.
She was assigned some medical specialists, like respiratory therapists and pediatricians, who work tirelessly to achieve their medical goals.
Due to her age, she was carefully monitored and assisted by several nurses. After about three to five days in the intensive care unit, her respiratory system was observed to improve, and she was also breathing perfectly well. She was discharged from the ICU setting in good condition.
Best Practice for Implementing Humidification
The use of a ventilator humidifier requires some procedures for the enhancement of general healthcare. To implement humidification, the following procedures are to be practiced:
- Determine Perfect Humidification Method: The selection of a perfect humidification method, either an active-passive humidifier or a heated humidifier, is vital for medical well-being.
- Monitor Temperature and Humidity: Constant checks should be taken on the appropriate level of humidity and temperature. This helps lessen inflammation and airway dryness and should be maintained according to patient demand.
- Sterile Water Utilization: Sterile Water is the best that can be used for airway humidification that won’t expose the patient to pollution or external factors.
- Routine Cleaning and Maintenance: To avoid microbial development and preserve ventilator maximum efficiency, rigorous adherence to proper upkeep and cleaning systems must be executed for various humidification components.
- Use of Heat and Moisture Exchanger Filters: These filters are a good component that helps to preserve humidity and also reduce infection tendency. The proper use of this filter will grant the body defense to external bodies.
- Sensor Check: When checking the degree of humidity consistently, the humidifier ventilator may automatically change settings with the help of an in-built sensor.
You can be a partaker of a respiratory system like no other with the aid of an advanced humidification system. This alternative breathing method is a type that brings more comfort, satisfaction and improved pulmonary treatment. However, you can also be a participant in this transformative respiratory care by taking a step today with a humidified ventilation system.
References
Advancement in Non-Invasive Ventilation
Dated to the 1940s, Non-invasive Ventilation has been undergoing a series of changes with various modifications in designs and techniques. This improvement in ventilator modes has exceeded imaginations and has brought a lot of technical healthcare solutions to diverse medical problems.
Evolution of Non-Invasive Ventilation Technology
NIV as a mode of ventilation has a great impact in the intensive care unit, as it provides a life-changing option that produces more positive outcomes. In addition, its impact on humanity is much more than an invention but one with immeasurable support and medical advancement that comes with a decrease in problems associated with intubation.
This article shall discuss some of the clinical importance of non-invasive ventilation in comparison with the invasive method, its impact on patient outcomes, its various technical and clinical benefits, alongside some of the future trends NIV possesses.

What’s Non-Invasive Ventilation?
One of the special modes of ventilation that does not require the use of a penetrating apparatus (endotracheal intubation) to aid respiration is known as Non-invasive ventilation (NIV). This is a unique method that is often employed to reduce complications associated with invasive ventilation eg. acute respiratory failure, airway disorder, etc. It is a technique with various forms of suitable designs and modifications that help in maintaining chronic respiratory conditions.
What Are The Clinical Benefits And Patient Outcomes of Positive Pressure Ventilation (NIV)?
Assisted ventilation in humans comes in various ways, one of which is the process of using positive pressure to aerate the lungs. This mode of ventilation is often called Positive pressure ventilation. In most cases, this method is always utilized in a non-invasive ventilation system with diverse advantages and benefits compared to others.

Medical Benefits and Technological Advancement of Non-invasive Ventilation
- Special Treatment Provision: Non-invasive ventilation in the healthcare system serves as a special equipment that is used for the treatment of diverse chronic and mild conditions. Oftentimes, this positive pressure ventilation device in the BiPAP method serves as a standard unique treatment method recommended for some specific respiratory failure and occasional health safety (OHS) e.g. AHRF, pneumonia, etc.
- Used for Obstructive sleep apnea: Due to NIVs’ evolving features (i.e. a developed user interface), it is often utilized in many chronic and acute respiratory cases such as the treatment of obstructive sleeping apnea (OSA). This evolution has produced facial and nasal means of breathing pressure (CPAP) aimed at treating sleep-related respiratory disorders.
- Chronic Respiratory Management: Currently, NIV is a ventilator mode used as a proven treatment for patients with COPD problems and related chronic respiratory problems like neuromuscular abnormalities.

Technological Advancement of NIV Ventilator Mode
- Advanced Human Interface: More effective mask designs that have stronger sealing qualities, and air-leakage reduction which improve patient comfort are some NIV distinct attributes. These features mostly allow usage by a wide range of patient demography (young babies, adults, pregnant women, etc.)
- Automated Monitoring System: With the help of a modern detector and monitoring system, it ensures an accurate pressure setting. This integrated detector also supplies real-time data collections that assist medical professionals to track patients’ progress and modify treatment plans.
- Telehealth Implementation: Some technical advancements in NIV ventilator mode such as telehealth integration have been an advantage for most healthcare providers to monitor their patient health status remotely.
Non-Invasive Ventilation Patient’s Outcome
The impact of non-invasive ventilation on life has gained remarkable attention and patients with a range of breathing complications have been greatly helped and their health alongside their quality of life have improved. Below are some patient outcomes of non-invasive ventilation:
- Enhanced Respirational Ability: Oftentimes, patients with respiratory complications after being placed on NIV positive pressure ventilation, usually have an improved ability to respire. Appropriate amounts of oxygen have been obtained and various breathing complications are lessened.
- Reduction in Death Rate: According to studies, the impact of these modes of ventilation on life has caused a considerable reduction in mortality rate. Most cases like COPD can be managed leading to auspicious survival results: an effect orchestrated by non-invasive ventilation initiation.
- Decreased Rates of Intubation: The use of positive pressure ventilation can help avoid or reduce the requirement for invasive ventilation mechanisms. Patients who avoid intubation face fewer of the risks that come with invasive procedures.
- Improved Comfort and Adherence of Patients: Non-invasive ventilation (NIV) offers a higher degree of patient comfort. It Improves patient compliance with recommended therapies and serves as a direct result of increased comfort, which guarantees long-term therapy advantages.
Clinical Advantages of NIV over Invasive Ventilation
Clinically and technically, Non-invasive ventilation has an edge over invasive ventilation. It possesses a lot of features that are of great remark. The advantages of non-invasive ventilation are beyond measures in the medical application and we have some as follows:
- Reduce cost: When considering extended hospital stays and the requirement for critical care services, NIV is frequently linked to decreased healthcare expenditures compared to invasive ventilation.
- Decreased Infection Risk: By doing away with intrusive procedures like intubation, Non-invasive ventilation lowers the risk of pneumonia and other ventilator-associated illnesses.
- Reduction in Barotrauma Risk: The risk of barotrauma, in which high pressure damages the lungs, exists with invasive respiration. However, diminished pressure settings in NIV lessen this danger and diminish the possibility of lung damage brought on by the ventilator.
- Promotes Oral Health and Communication: Compared to patients with endotracheal tubes, patients under NIV have greater ease of communication, eating, and oral hygiene, which improves patient wellness and overall quality of life.
- Use at home is possible: You can use the NIV mode of ventilation with no need for airway skills. Its usage requires less medical prowess compared to invasive ventilation.
Future Trends in Non-Invasive Respiratory Support
In the medical field, there are a series of expected developments in technological modifications of clinical equipment. One of these devices that has been a major concern is the non-invasive ventilator (NIV). This appliance has been an incredible device linked with improving patient outcomes with its possible future trends. These future trends are said to optimize ventilation settings and improve personalized healthcare, with the integration of exceptional features such as:
- Algorithm and Artificial Intelligence
- Portable Design
- Wearable device format
- Improved Telehealth System
- Biocompatible
- Enhanced User interface etc.
References
- https://pubmed.ncbi.nlm.nih.gov/19111105/
- https://rc.rcjournal.com/content/64/6/712
- https://breathe.ersjournals.com/content/9/5/338
- https://www.physio-pedia.com/Non_Invasive_Ventilation
- https://onlinelibrary.wiley.com/doi/full/10.1111/resp.13497
- https://www.ncbi.nlm.nih.gov/books/NBK578188/
- https://bmcpulmmed.biomedcentral.com/articles/10.1186/s12890-016-0289-y
- https://breathe.ersjournals.com/content/13/2/84
The Impact of Telemedicine on Critical Care
The emergence of telemedicine critical care sector has encountered an enormous change in the past few years. Its advent has brought a great change and alteration to the delivery of clinical care and access to specialized expertise. This great medical invention has also proven its essence with more patient outcomes as a result of its impact on medical consultation.
Telemedicine on Critical Care: A Modernize Care Impact
The effect of Telemedicine on critical care is an approach powered by technology, whose goal is centered on providing efficient medical treatment like remote patient monitoring, in the intensive care unit (ICU). Also, the introduction of a telemedicine network is to alleviate the increased scarcity of intensive care specialists and the escalating demand for telemedicine critical care services.
This article will provide you with telemedicine diverse opportunities and challenges in ICU, various transformative natures of telemedicine critical care for patients, and strategic integration of telehealth with traditional ICU practice.

Telemedicine in the ICU: Opportunities and Challenges
Telemedicine is an advanced health tech that has greatly influenced critical care – Telehealth-IUC. It’s a system that’s rapidly evolving, with faster adoption and use. Telehealth-IUC is built for more and with more expectancy, explore with me as we unfold some of its opportunities and concerns.
Telemedicine Opportunities in the Intensive Care
Technically and functionally, the impact of telemedicine on critical care has created diverse opportunities for integral care services and has gained remarkable recognition in the ICU. Some of these opportunities it provides are as follows:
- Quick Specialist Accessibility: With the help of telemedicine, intensive care patients have quick access to communicate with specialists at a remote distance to obtain specific knowledge. With quick specialist access, it enhances clinical settings most especially in urgent circumstances.
- Early Intervention and Decision-making: Telemedicine-IUC is a flexible system that possesses a great patient outcome caused by prompt intervention in a crucial expeditious setting. This flexible nature enables medical teams to quickly make decisions and communicate within themselves.
- Enhance Remote Monitoring: The impact of telemedicine in the intensive care units has granted medical professionals the ability to constantly monitor patients’ state of health remotely. It’s a very important element that can be used for neuromonitoring and with its immediate information seen to improve patient outcomes.

Various Challenges of Telemedicine Critical Care in ICU
With the high pace of telehealth development, standards, and healthcare advancement, some integral factors of great concern still need a touch of improvement. These various telehealth-ICU challenges are as follows:
- Security and Private Information Issues: Telemedicine in the intensive care unit involves the sharing of confidential patient data which are to be strictly protected and undisclosed. This patient’s information is to be secured with proper adherence to medical regulations.
- Need for Adaptation and Training: The need for a training program may be necessary for the proper utilization of telemedicine in the intensive care unit. Also, in some cases, there may be a slow rate of medical staff adaptation to the new tech system which may result in tactical change administration techniques.
- Technological Facilities Implementation; To utilize telehealth in the ICU effectively, a strong technological integration is greatly needed. The smooth implementation of technological facilities with telemedicine on critical care resources may cause some hurdles.
- Legal Barriers to Telemedicine Critical Care in ICU: Managing Medical Laws and Regulations may be difficult for an intensive care unit specialist. Telemedicine in the ICU for medical professionals has various barriers to conquer including the need for a license, liability concerns, and adherence to medical laws.

Case studies: Telemedicine Transforming Patient Care
The invention of telemedicine-ICU has played a great role in the transformative function of patient care. It’s earned a remarkable place in medical healthcare delivery with countless case studies over the past couple of years. Below are some case reports of telemedicine’s dramatic effect:
Case Study 1: Telemedic Urban Health Service Project
- Background: Cooperative action between a medical neuroscience group and telemedicine clinics aimed at extending the provision of healthcare services to remote areas with medical inequities.
- Application: The neuroscience group provides portable technological telemedicine devices that help people in these remote areas gain access to experts, become diagnosed, and consult medical professionals.
- Result: The application of telemedicine critical care in this area fosters prompt intervention, and advancement in accessibility and also aids patients easy access to specialists.
- Issues: some technical issues occurred due to limited network coverage which was scaled through with a satellite system.
- Conclusion: Telemedic Urban Health service provides extensive assistance to rural settlements with the help of telemedicine in critical care to break down distance barriers.
Case Study 2: Success in Managing Chronic Disease
- Background: A medical professional (intensivist) employed a telemedicine service to monitor a patient with chronic obstructive pulmonary disease (COPD). Aim to assist the patient in a post-surgery maintenance process.
- Application: The intensivist constantly reaches his patient via a telemedicine device to provide further instruction and monitoring guidelines about Non-invasive ventilation.
- Result: A successful patient outcome occurred as a result of the patient’s increased control rate. An increase in medical compliance and good health with continuous monitoring treatment.
- Issues: Corrective instructions and NIV device adjusting guidelines are done by the patient, obstructive network coverage causes a breakage in communication.
- Conclusion: The application of telemedicine devices causes effective chronic disease maintenance with the doctor having more opportunities to save lives remotely.

Strategies for Integrating telemedicine with traditional ICU practice
Telemedicine in critical care has been a dynamic invention in the healthcare system that serves as a technical means of providing solutions for optimum patient care. It is a medical-tech innovation that can be integrated with traditional ICU practices to produce more patient outcomes. Below are some strategic ways of telemedicine-ICU integration:
- Remote Telemonitoring Application: Employ the use of a reliable patient monitoring application that will provide a remote health indicator for the intensivist. With the help of this telemonitoring system, ICU personnel can obtain current information that will allow prompt medical care.
- Modified Tele-ICU Procedure: Create a specialized procedure that allows easy incorporation of telemedicine with the ICU’s current procedures. Carefully dish out the responsibilities of each healthcare provider; either in remote settings or at the alpha location.
- Ensure Teleconsultation Provision: To protect patient data confidentially, facilitate the provision of a remote consultation with expertise, and ensure a more secure texting app and teleconferencing to improve coordination and knowledge sharing.
- Team Education and Training: Medical teams are to be equipped with telemedicine-related competencies. Also, funding for initiative training to teach intensivists about all telemedicine entails.
- Families and Patient Involvement: Employ various techniques that will encourage patients and their families to partake in virtual intensive care communication, allowing openness and assistance in emergency times.
- Multidisciplinary Cooperation: Develop a strong interaction among the telemedicine-ICU personnel e.g. physicians, specialists, ICU personnel, and lots more.
The impact of Telemedicine on critical care has been an advanced technological solution incorporated into the medical sector for the increase of patient outcomes in ICU and generally the improvement in the healthcare system. Telehealth-ICU entails a wide range of opportunities and challenges but with a strategic implementation into traditional ICU practice, it radiates its essence as a transformative component of patient care.
You can explore the incredible impact of telemedicine in contemporary healthcare today and discover a transformative remote patient outcome. Join the latest healthcare innovation today, and witness medical solutions at your comfort.
References
How to Navigate the Challenges of Medical Device Procurement?
One of the integral factors that divine the proper regulation of health and effective distribution of service in a healthcare sector is its medical device procurement. This is a vast field in medical care that encompasses the purchase of medical devices, commodities, goods, machinery, and even the commission of healthcare structures development.
In some cases, most healthcare organizations grant limited attention to the impact of medical procurement. Yet, many healthcare factors and also medical treatments are greatly influenced by medical device procurement. To create an efficient medical distribution and management, some set of challenges need to be overcome. Although, it’s not simple to navigate medical device procurement challenges.
Many times, medical personnel encounter a wide range of challenges to obtain the facilities needed for productive patient treatments that range from supply network delays to intricate rules and regulations. In this article, we will be taking a deeper look into the key considerations in medical device selection, strategies for cost-effective procurement, and tips for building strong relationships with suppliers.
Key Considerations in Medical Device Selection
Looking into the aspect of medical device selection during procurement, there are likely risks at the clinical stage that are bound to occur but at a considerable degree. To minimize device risk intensity, some key factors are to be considered when selecting a medical device. Fasten your seat, as we explore these factors together:
Compliance with Functions and Regulations
A major factor that should be put into consideration is the ability of a medical device to fulfill its functional purpose. Also, It is crucial to confirm the medical device regulatory compliance and if been approved and granted the required certificate from medical agencies eg. FDA, CE, WHO, etc.
Economic Viability
While considering every other factor, one of the key elements to be evaluated is the device cost and total expense. However, the economic viability of a device should not only center on its cost but also a great consideration of its improvement possibilities, impact on patient outcome, and functional efficacy.
Device Production and Design
There are countless manufacturers in the healthcare sector that are known for the type of product they produce. Knowing the manufacturer’s reputation is an integral factor that helps in understanding the quality of the producer and its product. Also, proper examination of the device’s artistic or cosmetical nature should be considered.
Device Orientation and Usability
Mostly when it comes to medical devices like imaging machines, operating machines, surgical supplies, etc. a very important factor to consider is the easy accessibility and usage of the device. A proper orientation program about the operation of the device is essential and a good user-friendly interface is to be selected.
Device Lifespan
When choosing a medical device, its durability and quality are of great consideration. Often, the lifespan of a device is to be considered with the importance of its usage. For instance, a device like an imaging machine with a guarantee of three years is less durable compared to that of a lifetime.
Device Compatibility
A detailed outline of the medical device’s intended usage must be determined and its ability to integrate with the current medical facilities is to be evaluated. It is also important to determine the device’s biocompatibility when in close contact with tissue. As it prevents possible medical device complications and danger to a patient.
Strategies for Cost-Effective Procurement
In today’s rapidly evolving healthcare landscape, optimizing procurement strategies for medical devices has become more crucial than ever. Here are some essential tactics to consider for cost-effective procurement:
Systematic Source of Supplier
Before the purchase of any medical device, a systematic approach and analysis of sources to obtain your desired gadget are to be considered. This strategy provides a competitive atmosphere and perhaps results in a favorable price and conditions.
Tech Procurement Approach
The use of technology in the aspect of medical device procurement cannot be sidelined. It’s a means that improves productivity and efficiency and also lessens mistakes by eradicating the need for manual operations. You can access the market for software and tools that will aid your exploration program.
Creating Scale of Preference
The projection of the needs of various devices with the range of demand is to be taken. This can be done by gathering and evaluating information from previous purchases and patterns. A scale of preference is needed to maintain the proper quality of supplies.
Effective Negotiation with Suppliers
A tactical approach to medical device procurement cost-effect is in the negotiation of beneficial rates and conditions. Creating a mutually beneficial dialogue with your supplier is one of the foremost vital components that can aid effective device bargaining.
Relationship Management with Suppliers
Through reciprocal trust and respect, a solid relationship with suppliers can be created. This rapport can improve medical device transaction performance and more favorable conditions can be established.
Risk Management
There are various inevitable risks associated with purchasing medical devices. However, consulting an effective strategy for the management of this risk can help stop unforeseen expenditures and financial problems.
Quality Valuation
The quality and versatility of a device must be considered and prioritized when procuring medical devices. With the help of a quality valuation, likely faulty devices and associated expenses are eradicated.

Tips for Building Strong Relationships with Suppliers
Many people often minimize the importance of suppliers without realizing what a big role they play. Any business that wants to expand must have a reliable supplier and have a friendly relationship with them. Below are some tips for building a strong supplier rapport:
- Create good communication skills with the display of clear and consistent conversations to enhance transparency and trust.
- Share your purpose and ensure alignment in goals with your supplier.
- Schedule constant and punctual meetings with your supplier to talk about performance, and pressing issues and also discuss areas that need development.
- Ensure to always make payments to your suppliers on time as this creates trust and dependability.
- Provide helpful remarks on goods or services to your supplier and also urge your supplier to do the same.
- Regard your supplier not just as your business associate but as a strategic ally as well
- While bargaining, bargain with respect and professionalism to keep the relationship strong and steady.
- One of the key components of building a strong supplier relationship is trust. Trust is built with complete sincerity in goals and sharing of problems. Also when building trust, ensure to be loyal completely all along the way.
- In a business, disputes and certain issues are bound to occur. However, it is advisable to resolve every dispute amicably with respect and professionalism.

Biosys: A Trusted Partner in Medical Device Procurement
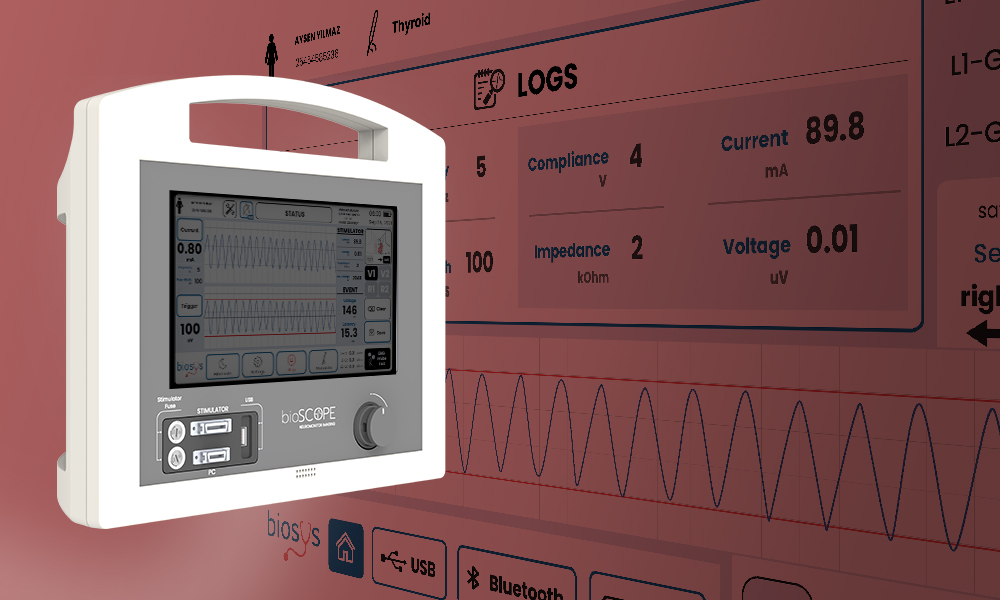
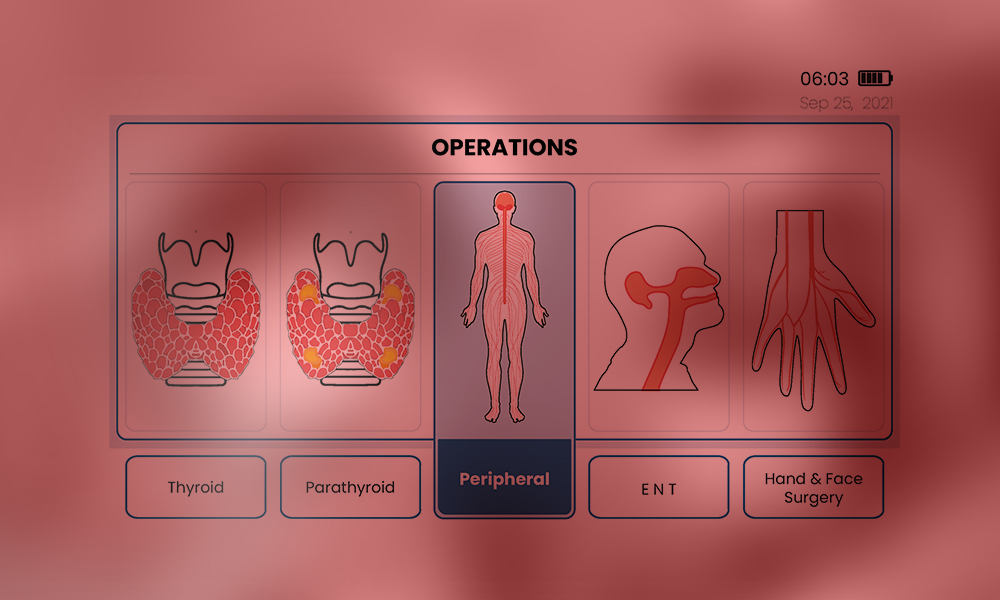
At Biosys, we take pride in being a reliable partner for our clients, demonstrating our commitment to excellence across all aspects, including Biyovent, BioAqua, BioScope, and Bio2Flow. As a supplier, we firmly stand behind the quality and functionality of these critical healthcare devices. At Biosys, we thoroughly understand the challenges that suppliers face in the medical device procurement process, and we are committed to making our clients’ jobs easier.
Our focus on providing top-notch products revolves around ensuring that our medical devices meet the objectives required by the healthcare sector, comply with regulatory standards, and obtain necessary certifications from organizations such as CE, WHO, and others. Additionally, we prioritize “Economic Viability,” evaluating the cost and overall expenses of our devices while considering their potential for improvement, impact on patient outcomes, and functional efficacy.
Another crucial aspect is “Device Production and Design,” where our goal is to facilitate the ease and effectiveness of healthcare professionals (doctors, nurses, etc.) in using our devices, making their jobs more manageable. “Device Orientation and Usability” is emphasized, especially for intensive care equipment, ensuring easy accessibility and user-friendly interfaces. When it comes to “Device Lifespan,” durability and quality are our primary considerations, and we offer extended warranties for our devices. Furthermore, “Device Compatibility” is thoroughly evaluated to determine how well our medical devices integrate with current healthcare facilities, preventing potential complications and ensuring patient safety.
Biosys is not just a supplier; we are your committed partner in achieving success and efficiency in your medical device procurement endeavors, offering support that goes beyond the transaction.
Discover the Biosys difference and explore our innovative and reliable healthcare solutions that meet the highest standards of quality, functionality, and usability. Whether you need solutions for an Intensive Care Mechanical Ventilator with Biyovent, Ventilator Compatible Humidifier with BioAqua, Intraoperative Neuromonitoring with BioScope, or High-Flow Oxygen Therapy with Bio2Flow; Biosys will provide the solutions you need in the specified areas.
References
Breathing Easy: The Crucial Role of Humidification and Temperature Control in Respiratory Care
Humidity and temperature control have long been standard care procedures in mechanical ventilation. It has been stated in many articles published over the years that dry gases damage the airways. For this reason, external humidification and heating devices are used in respiratory care to tolerate the lack of natural humidification factors. Reservoirs, wires, heating devices and other systems have become standard equipment in intensive care units.
Controlling Humidity and Temperature in Respiratory Care
One of the important functions of the respiratory system is to ensure heat and moisture exchange in the inhaled air. The nasal connective tissue, which is the first organ of inspiration, has many capillaries. These are responsible for increasing the moisture-carrying capacity of the inhaled air by heating it.
The air passing through the nose and descending into the respiratory tract reaches a temperature of 37°C and 100% relative humidity. Cells in the respiratory tract maintain the mucosal layer, which traps pathogens and is an interface for moisture exchange. However, moisture capacity is more limited in the lower respiratory tract. Therefore, poor humidification after endotracheal intubation causes potential damage to the respiratory epithelium; this is manifested by increased work of breathing, atelectasis, thick and watery secretions, and cough and/or bronchospasm.
While it is controversial whether additional heat and humidity are always necessary in cases such as non-invasive mechanical ventilation where the upper airway is not bypassed, active humidification is always recommended. Active or passive humidifier systems are used in patients on mechanical ventilation.

The Importance of Maintaining Proper Respiratory Care Conditions
While humidification is mandatory in tracheostomy or intubated patients, this is optional in non-invasive ventilation. Humidifying the airway of a patient under ventilation support is one of the important interventions of the intensive care process. An inappropriate humidifier type and setting can damage the airway and increase respiratory workload, leading to adverse outcomes. The choice of humidifier may vary depending on clinical situations, and healthcare professionals should be aware of its advantages and disadvantages when choosing the appropriate medical devices.
Challenges In Achieving Optimal Conditions
Respiratory care’s dynamic and diverse nature creates challenges in achieving optimal conditions. Traditional methods frequently lack the precision required to tailor conditions to the needs of individual patients. Variations in environmental factors, patient-specific requirements, and the requirement for real-time adjustments add to the difficulties. Inconsistent humidity and temperature control can result in discomfort, poor therapeutic outcomes, and a higher risk of respiratory complications.
Solutions for Keeping Good Conditions
Innovative solutions in healthcare technology, such as the Bioaqua humidifier, address the challenges of maintaining proper respiratory care conditions. These devices include various features designed to optimize humidity and temperature levels, resulting in a comfortable and practical therapeutic environment for patients.
Bioaqua’s adjustable humidity control settings enable healthcare providers to tailor treatment plans to individual patient requirements. Incorporating innovative technology allows for remote monitoring and adjustments, allowing for a more proactive approach to patient care. The device’s user-friendly interface makes it accessible to healthcare professionals and patients, improving the overall respiratory therapy experience.
The Bioaqua humidifier has temperature control that is seamlessly integrated and maintains an optimal temperature range. This is achieved by utilizing advanced heating elements and thermal control systems. These technical features work together to help the device provide a tailored and responsive approach to humidity and temperature control in respiratory care.
Impact on Respiratory Conditions Examples
COVID-19 patients are among the patient groups for which invasive or non-invasive ventilation is most frequently used. Kumar et al. (2021) recommend in their article that active heat and humidification improve functions by clearing secretions from the airway in COVID-19 patients. They stated that this increased the patient’s comfort and improved NIV tolerance.
A study was conducted in 2020 to evaluate whether heated humidified ventilation could improve the prognosis in normothermic thoraco-abdominal aortic aneurysm repair operations. In this study, patients were divided into two group: the group using heated ventilation and water blankets and the group using water blankets only. Intraoperative core temperature, coagulation functions and in-hospital mortality were analyzed in the study. As a result, less blood loss, anti-coagulant dose and in-hospital mortality were observed in the heated and humidified ventilation group.
Respiratory care is extremely important, especially in newborns. A study conducted in 2015, which investigated the effect of adding heated and humidified gas to the treatment during birth and newborn arrival on body temperatures in premature babies, showed that humidification is more effective in preventing hypothermia.

The Role of Bioaqua Humidifiers in Innovative Solutions
Bioaqua stands out as an innovator in the humidification device market. Bioaqua humidifiers are designed with advanced technologies to control humidity levels precisely, ensuring optimal patient therapeutic conditions. These devices include adjustable humidity settings, real-time monitoring, and adaptive algorithms that cater to the user’s needs. Smart technology integration enables healthcare providers to monitor and adjust settings remotely, promoting a more personalized and responsive approach to patient care.
The Bioaqua humidifier incorporates temperature regulation, addressing the challenges associated with temperature control in respiratory care. The device maintains a precise temperature range, reducing the risk of complications caused by high temperatures. Bioaqua is an invaluable asset in the respiratory care landscape due to its comprehensive approach to humidity and temperature control.
Collaboration in the Development of Effective Solutions
The advancement of advanced humidification devices such as Bioaqua demonstrates the value of collaboration among respiratory therapists, clinicians, and technology experts. These collaborations result in devices that not only meet the immediate needs of patients but also pave the way for continuous improvement in respiratory care by combining clinical expertise with technological innovation.
Incorporating the perspectives of respiratory therapists and clinicians ensures that the technology meets the practical needs of healthcare settings. The collaboration of medical expertise and technological innovation is critical for developing devices that are user-friendly, adaptable, and capable of addressing the wide range of challenges posed by respiratory conditions.
Balancing Humidity And Temperature: An Essential Factor In Respiratory Care
Harmony between humidity and temperature control is critical for patient well-being and therapeutic success in the intricate dance of respiratory care. Bioaqua humidifiers are the pinnacle of innovation in this field, with advanced features designed to meet patients’ and healthcare providers’ changing needs.
While navigating the complex landscape of respiratory health, it is clear that collaboration among respiratory therapists, clinicians, and technology experts is critical in developing effective solutions. The Bioaqua humidifier exemplifies what can be accomplished when expertise and innovation come together to create devices that revolutionize respiratory care.
We invite you to visit our website to learn more about the transformative capabilities of Bioaqua humidifiers and to experience firsthand the benefits of advanced therapeutic humidity and temperature control in pulmonary care. Take the first step towards breathing easier and learn how Bioaqua can make a difference in the lives of those who require respiratory support.
Allow Bioaqua to assist you in your pursuit of optimal respiratory health.
If you would like to get detailed information about this revolutionary device, you can browse our catalogue and get the details from the link. For our other products, follow the link.
References
- Al Ashry HS, Modrykamien AM. Humidification during mechanical ventilation in the adult patient. Biomed Res Int. 2014;2014:715434. https://doi: 10.1155/2014/715434.
- Michael P. Meyer, David Hou, Nazmul N. Ishrar, Ingrid Dito, Arjan B. te Pas, Initial Respiratory Support with Cold, Dry Gas versus Heated Humidified Gas and Admission Temperature of Preterm Infants, The Journal of Pediatrics, Volume 166, Issue 2,2015, Pages 245-250.e1, https://doi.org/10.1016/j.jpeds.2014.09.049.
- Ruben D Restrepo and Brian K Walsh, Humidification During Invasive and Noninvasive Mechanical Ventilation: 2012, Respiratory Care May 2012, 57 (5) 782-788; DOI: https://doi.org/10.4187/respcare.01766
- Rui Zhao, Jiawei Qiu, Jinlin Wu, Wenxiang Jiang, Enzehua Xie, Wei Gao, Cuntao Yu, Juntao Qiu, Effect of heated humidified ventilation on intraoperative core temperature and prognosis in normothermic thoraco-abdominal aortic aneurysm repair, Journal of Thoracic Disease, 2020, Vol 12, No 3 (March 23, 2020), doi: 10.21037/jtd.2020.01.61
- Amarjeet Kumar, Chandni Sinha, Abhyuday Kumar, Neeraj Kumar, Ajeet Kumar, Kunal Singh, Prabhat Kumar Singh, Inefficient humidification as the cause of noninvasive ventilation failure in COVID-19 patients, Brazilian Journal of Anesthesiology (English Edition), Volume 71, Issue 6, 2021, https://doi.org/10.1016/j.bjane.2021.07.021.
Innovative Approaches: High-Flow Oxygen Therapy in the ICU
Intensive Care Unit (ICU) is different, whereby individuals suffering from acute and critical respiratory conditions demand complex assistance. Mechanical ventilation has proved crucial for the medical care of these cases for decades. Mechanical ventilators are frequently used in pathological situations such as low oxygen levels or high carbon dioxide levels where the patient has difficulty breathing. Nevertheless, over recent years, there appears to be a new therapeutic way called high-flow oxygen therapy, which is likely to substitute or serve with traditional respiration practices. The goal is to create a particular focus on optimizing humidification to enhance patient comfort and respiratory support.
High-Flow Oxygenation (HFO)
In clinical applications, oxygen therapy can be given as low flow (with mask or nasal cannula) or high flow (Venturi mask or nonrebreathers). However, in conventional methods, some of the oxygen inhaled by the patient is not delivered completely. Since the oxygen is not heated and humidified, the patient may not tolerate it for long periods. High-flow oxygen therapy, which is mainly used for respiratory diseases in pediatric patients, has found a serious place, especially in the COVID-19 pandemic and has begun to be widely used in adult patients as well.
High-flow oxygen/cannula therapy is gaining widespread attention as an alternative approach to respiratory support in intensive care patients. This method is applied via air or oxygen mixer (rate up to 60 L/min at 21% to 100% oxygen fraction), humidifier, patient circuit and nasal cannula. The high-flow, warmed, humidified oxygen removes carbon dioxide from the anatomical dead space, making breathing easier and increasing patient comfort.
Benefits of HFO in ICU
The benefits of HFO go further than simple improvement in gas exchange. Compared to traditional mechanical ventilation, HFO offers numerous advantages:
- Comfortable for patients: The nasal prongs are soft and small. Several studies stated that patient comfort is higher with HFNC than with a conventional nasal cannula or face mask
- Warming and humidification of secretions: There is no chance for warming and heating oxygen when applying with a nasal cannula or face mask. In HFNC, oxygen is humidified and warmed before being administered to the patient. This increases the patient’s ability to tolerate treatment over a long period. This can facilitate the removal of mucus and other secretions from the airway.
- PEEP effect: Although the HFNC is an open system, the high-flow nasal cannula provides resistance to expiratory flow and increases airway pressure. PEEP decreases lung compliance, residual capacity reduction and elimination of refractory hypoxia. PEEP allows collapsed lung alveoli to open. It improves oxygenation and lung compliance.
- High flow rate: Access to 60 L/min oxygen flow, which is not possible with normal oxygen devices, is possible with HFNO devices. Flow rate, humidity and temperature can be adjusted with the device. This allows the treatment to be adapted to the individual’s condition, increasing effectiveness.
Mechanism Of Action And Clinical Applications
Nasal high-flow therapy contributes to improving the fractionation of alveolar gases by reducing nasopharyngeal dead space. The expandability of the nasopharynx provides significant inspiratory resistance relative to expiratory effort.
HFNO provides adequate flow rates to accommodate inspiratory flow and thus significantly reduces the inspiratory resistance associated with the nasopharynx and thus eliminates the associated work of breathing. Delivery of heated and humidified oxygen to the respiratory organs increases pulmonary compliance and reduces metabolic load compared to dry and cold gas. The high flow in the nasopharynx provides positive tensile pressure to activate the lungs.
High flow oxygen therapy indicates for hypercapnic respiratory failure, hypoxemic respiratory failure, post-extubation, preintubation oxygenation, acute heart failure and sleep apnea. In pediatric patients, it is mainly indicated for bronchiolitis, but also for pneumonia, croup, asthma and post-extubation.

Patient-Centered Care and Comfort
Patient comfort and satisfaction in the rigorous conditions of the ICU are critical aspects of providing quality health care. From the patient’s perspective, HFO significantly reduces discomfort associated with traditional mechanical ventilation.
- Reduced Discomfort: A soft nasal cannula and gentle airflow take away distress caused by the endotracheal tube, making patients more tolerant and less anxious.
- Improved Communication: Additionally, the methodology enables patients to communicate freely with each other during their stay, which facilitates an improved atmosphere.
- Enhanced Sleep Quality: Compared to mechanical ventilation, HFO allows for better rest and, consequently, better recovery of patients because it is less noisy and does not cause disruption.
Clinical Outcomes and Cost-Effectiveness
HFO therapy has been studied extensively and proven clinically beneficial. One of the most comprehensive studies investigating the effectiveness of nasal high-flow therapy is the Clinical Guideline published by the American College of Physicians. According to this guideline, compared to NIV, it has been shown to improve clinical outcomes as an initial treatment for acute respiratory failure and improve patient comfort by reducing re-intubation compared to standard oxygen therapy. It is stated that it causes fewer complications in patients than NIV or COT.
The effectiveness of HFNO in patients with hypoxia in acute heart failure was investigated in a retrospective cohort study. It has been stated that there is a better improvement in left ventricular parameters in patients receiving HFNO treatment compared to non-invasive positive pressure ventilation. It has been concluded that HFNO may be an ideal model, especially in hypoxemic AHF patients.
In another meta-analysis investigating the use of HFNO in anesthesia induction, it was compared with FMV. The use of HFNo for anesthesia induction has been shown to significantly improve oxygenation compared to FMV.
In addition to those mentioned above, many scientific studies are showing the effectiveness of HFNO.
Cost Savings
In a study conducted in England, the cost-effectiveness of HFNO use was investigated. Three different cost-effectiveness models were used in this study: the pre-intubation model and the post-extubation model in low-risk and high-risk patients. The use of HFNO in first-line treatment is reported to provide estimated savings of £469 per patient compared to standard oxygen therapy and £611 compared to NIV. NHF cost savings for the high severity subgroup were found to be £727 compared to standard oxygen and £1,011 compared to NIV.
For post-intubation low-risk patients, NHF provides an estimated cost saving of £156 compared to standard oxygen. The savings for post-intubation high-risk patients was stated to be £104.
Another study in infants with bronchiolitis compared low-flow oxygen therapy and HFNO therapy. In this study, treatment costs were found to be between $1786-3600 for HFNO, while these figures were found to be between $2175-5125 for standard treatment. Based on this, the cost-effectiveness of high-flow oxygen therapy can be demonstrated.

Introducing Bio2Flow: Your Partner in High-Flow Oxygen Therapy The Right Way
Giving a significant gain to the medical device world with Biyovent, an Intensive Care type mechanical ventilation device, Biosys continues to produce new device solutions for the sector. BiO2Flow, a high-flow oxygen therapy device, is a revolutionary device.
If you would like to get detailed information about this revolutionary device, you can browse our catalogue and get the details from the link. For our other products, follow the link.
References
- Walter K. Mechanical Ventilation. JAMA. 2021;326(14):1452. doi:10.1001/jama.2021.13084
- Heated and humidified high-flow nasal oxygen in adults: Practical considerations and potential applications, Robert C Hyzy, MD, Uptodate, Access time: Dec 2023
- Huiying Gao, Lin Chen, Xiaofei Kang, High-Flow Nasal Cannula Oxygen Therapy in Patients With Acute Heart Failure: A Meta-analysis, The Journal for Nurse Practitioners, Volume 19, Issue 5,2023, https://doi.org/10.1016/j.nurpra.2023.104602.
- Nishimura M. High-Flow Nasal Cannula Oxygen Therapy in Adults: Physiological Benefits, Indication, Clinical Benefits, and Adverse Effects. Respir Care. 2016 Apr;61(4):529-41. doi: 10.4187/respcare.04577. PMID: 27016353.
- Toffaletti JG, Rackley CR. Monitoring oxygen status. Adv Clin Chem 2016;77:103-24.
- Emily Eaton Turner &Michelle Jenks (2017), Cost-effectiveness analysis of the use of high-flow oxygen through nasal cannula in intensive care units in NHS England, https://doi.org/10.1080/14737167.2018.1411804
- Paula Heikkilä MSc, Leena Forma PhD, Matti Korppi MD, PhD (2016), High-flow oxygen therapy is more cost-effective for bronchiolitis than standard treatment—A decision-tree analysis, Pediatric Pulmonology, https://doi.org/10.1002/ppul.23467
- Kevin Dysart, Thomas L. Miller, Marla R. Wolfson, Thomas H. Shaffer, Research in high flow therapy: Mechanisms of action, Respiratory Medicine, Volume 103, Issue 10,
- 2009,Pages 1400-1405, https://doi.org/10.1016/j.rmed.2009.04.007.
- Baldomero, A. K., Melzer, A. C., Greer, N., Majeski, B. N., MacDonald, R., Linskens, E. J., & Wilt, T. J. (2021). Effectiveness and Harms of High-Flow Nasal Oxygen (HFNO) for Acute Respiratory Failure: An Evidence Report for a Clinical Guideline by the American College of Physicians. Annals of Internal Medicine, 174(7), 952. https://doi.org/10.7326/M20-4675
- Song, Jl., Sun, Y., Shi, Yb. et al. Comparison of the effectiveness of high-flow nasal oxygen vs. standard facemask oxygenation for pre- and apneic oxygenation during anesthesia induction: a systematic review and meta-analysis. BMC Anesthesiol 22, 100 (2022). https://doi.org/10.1186/s12871-022-01615-7
- Tong, Xiao MDb; Tong, Ningning MDa; Yao, Feifei MDc; Yan, Jing MDd; Ci, Caizhe MDd,*. Clinical outcomes of high-flow nasal cannula oxygen therapy in acute heart failure patients with hypoxemia: A retrospective cohort study. Medicine 101(43):p e31124, October 28, 2022. | DOI: 10.1097/MD.0000000000031124
What are the 4 Different Types of Medical Ventilators?
Currently, there are different types of ventilators offered to patients by health units in accordance with the patient’s needs. Depending on the particular circumstances, ventilators can be typed according to where the treatment needed by the patient has been applied and how it is applied; these types are as follows: ICU ventilators, Home ventilators, Ambulatory and Emergency ventilators, and Anaesthesia ventilators. This article covers various types of medical ventilators.
ICU Ventilators
Generally named after where they are mainly used, ICU ventilators are typically the most advanced and critical care ventilators. They are used in ICU settings in hospitals and health facilities, for the most serious patients and with the most severe respiratory conditions.
These sophisticated machines offer many modes differing to condition and illness: volume assist/control (v- A/C), pressure assist/control (p- A/C), pressure support ventilation (PSV), synchronized intermittent mandatory ventilation with volume support (vSIMV) and synchronized intermittent mandatory ventilation with pressure support (p-SIMV. (1)
With one variable, only ventilation can be applied. Still, ICU ventilators have dual control (of both volume and pressure). An ICU ventilator uses both variables, volume, and pressure, to present ideal breath to patients.
In addition, to the expected need for wide monitorization and control mechanisms in ICU patients, an ICU ventilator has wide settings menu, interface, and dedicated keys that are more complex than other ventilator types. (1) ICU ventilators present FiO2 sensors and large displays, particularly for breath rate, Peep Inspiratory Pressure, and exhaled tidal volume monitorization. They also have more complex and better secure locks and alarm systems.
Home Ventilators
The name can easily understand as home ventilators or home care ventilators; they are mechanical ventilators designed to serve the patient’s needs at home or in other places like palliative support facilities. (2) These ventilators should be simple because they can be used by people who are not trained as much as a health care practitioner or a clinician. Also, these ventilators should be complex simultaneously because they have some features of highly sophisticated ventilators; for a better-using home, ventilators have a non-complex interface, an easily operatable system, and minimal accessories. They are the most fitted ventilators for a patient’s breathing needs at home with a short trigger time. (3) And they are also tough machines with low costs. Patients with respiratory failure, chronic obstructive pulmonary disease (COPD) (4), amyotrophic lateral sclerosis (ALS), restrictive lung disease, congenital muscular dystrophies, etc., can be put on home ventilator care.
Ambulatory and Emergency Ventilators
These are breathing devices deployed at short notice for patients in emergency or/and when they need to be transferred from one place to another to their medical condition. These are self-contained, compact, and sturdy ventilators for the most challenging weather and other circumstances. In some cases, Ambulatory and Emergency ventilators can use them for the post-operative care of patients. These ventilators feature technological developments that are as close as possible to modern ICU ventilators.
Anesthesia Ventilators
These ventilators are typically employed in surgery room settings for patients who are undergoing a surgical operation and/or to help them to breathe during the post-op period to recovery. (5) They are more limited than ICU ventilators in the range of ventilatory settings and monitoring features. Again, anesthesia ventilators allow most, but not all, features present in an ICU ventilator. Typically, they have volume-controlled (VCV) and pressure-controlled (PCV) modes. However, besides the conventional types, modern anesthesia ventilators today present newer modes of ventilation such as synchronized intermittent mandatory ventilation (SIMV) and pressure support ventilation (PSV). (6)
Therefore, these are different types of ventilators offered to patients by health units in accordance with the patient’s needs. Depending on the particular circumstances, ventilators can be typed according to where or how it is applied. However, it is essential to remember that most of these ventilators have certain superimposed features. Obviously, on facing any respiratory problem that is mild or severe, the user or applier should seek advice from experts about which type of ventilator is appropriate to use. Indeed, experts’ recommendations should be followed.
Discover the ultimate choice in smartwatch bandjes and horlogebandjes at our online store! Elevate your style with our premium selection of horlogebandjes designed to complement your smartwatch perfectly. Upgrade your look effortlessly with our range of horlogebandjes for every occasion.

Let’s Meet with Biyovent ICU Types of Mechanical Ventilator
Biyovent ICU Ventilator makes a difference in the ventilation process with its unique specifications. Biyovent has been carefully thought out with every detail of the ventilators and developed with a holistic approach. Prepared for mass production in cooperation with Arçelik, Baykar, and Aselsan.
What are some specific features of Biyovent?
- Invasive and Non-invasive Ventilation
- Integrated Nebulizer
- High Flow Oxygen Therapy
- Suitable for Pediatric, Adult and Newborn (Optional) Patients
- Smart Ventilation Modes
Learn more details about Biyovent ICU Ventilator
Get in contact with Biosys Sales Team
References
1 – Chatburn, R. L., El-Khatib, M., & MirelesCabodevila, E. (2014). A taxonomy for mechanical ventilation: 10 fundamental maxims. Respiratory care, 59(11), 1747–1763. https:// doi.org/10.4187/respcare.03057
2 – Simonds A. K. (2006). Risk management of the home ventilator-dependent patient. Thorax, 61(5), 369–371. https://doi.org/10.1136/ thx.2005.055566
3 – Grassion, L., Llontop, C., Layachi, L., Hubert, E., Morelot-Panzini, C., & Gonzalez-Bermejo, J. (2018). Définitions des paramètres de ventilateurs de domicile [Home care ventilator’s settings]. Revue des maladies respiratoires, 35(9), 992–996. https:// doi.org/10.1016/j.rmr.2017.04.004
4 – Ambrosino N, Vagheggini G. Non-invasive ventilation in exacerbations of COPD. Int J Chron Obstruct Pulmon Dis. 2007;2(4):471-476.
5 – Coisel, Y., Millot, A., Carr, J., Castagnoli, A., Pouzeratte, Y., Verzilli, D., Futier, E., & Jaber, S. (2014). How to choose an anesthesia ventilator?. Annales francaises d’anesthesie et de reanimation, 33(7-8), 462–465. https:// doi.org/10.1016/j.annfar.2014.07.006
6 – Cameron, P. D., & Oh, T. E. (1986). Newer modes of mechanical ventilatory support. Anesthesia and intensive care, 14(3), 258–266. https://doi.org/10.1177/0310057X8601400306
What is Respiratory Care: Trends and Advancements
Patients with severe respiratory disorders frequently require specialized care in the Intensive Care Unit (ICU), a vital area in healthcare. The field of respiratory care advances in tandem with medical science. The future of respiratory care is closely tied to virtual care technology. As we explore changes in respiratory health, it’s clear that new and improved virtual care solutions are shaping how we approach diagnosis and treatment.
This blog explores cutting-edge developments in respiratory care that have the potential to completely transform the way we diagnose, manage, and treat respiratory conditions.
ICU In The Context Of Respiratory Care
A cooperative team of medical experts, comprising doctors, nurses, and the vital respiratory therapist, collaborates in the dynamic Intensive Care Unit (ICU) to deliver unmatched care to patients in critical condition. Their proficiency encompasses various tasks, including complex ventilator control, diagnostic blood drawing, and bronchoscopy support. Specialized gas administration including treatments such as heliox and nitric oxide and careful attention to every aspect of hemodynamic monitoring highlight the respiratory therapist’s vital roles in this high-stakes setting. [1]
Respiratory Care Personalized Medicine
Personalized medicine is a cutting-edge approach that customizes medical treatments based on a person’s genetic composition, lifestyle, and surroundings. It refers to creating respiratory care plans specially tailored to every patient’s requirements. Pharmacogenomics, which identifies the safest and most effective drugs for specific patients, is one possible example. Genetic differences can affect a person’s response to a drug, so adjusting a medication’s dosage could significantly improve treatment results.
Wearable technology developments are crucial for real-time patient monitoring, respiratory pattern data collection, and individualized interventions or feedback. Intelligent inhalers, which track medication compliance and offer instantaneous feedback, are invaluable for treating respiratory ailments. Pulmonary function tests are easily accessible with portable electronic spirometers, which close the gap between patient monitoring and diagnosis. Furthermore, digital stethoscopes that use artificial intelligence (AI) improve lung auscultation accuracy and offer useful diagnostic information. [2]
Machine Learning and AI in Radiation Therapy
Significant progress is being made in changing respiratory care through artificial intelligence (AI) and machine learning (ML). These technologies are adept at analyzing vast datasets with unprecedented speed and accuracy, offering clinicians valuable insights for treatment planning and decision-making. They help optimize ventilator settings for individual patients to predictive analytics for early disease detection.
AI is a valuable tool in predicting disease progression, enabling medical professionals to customize treatment regimens and interventions to improve patient outcomes. By utilizing extensive biological and clinical datasets, these technologies provide priceless insights for forecasting outcomes, individualized treatment planning, and disease prediction. One prominent example is the application of AI algorithms to the analysis of medical imaging, including CT and chest X-rays, for the early diagnosis of respiratory disorders. Diagnoses can be made more quickly and accurately thanks to these systems’ ability to spot irregularities and subtle patterns that the human eye might miss. [3]
How does AI help respiratory medicine?
The revolutionary collaboration of AI, ML, and respiratory medicine advances our knowledge of disease mechanisms, expedites drug development, and improves personalized therapies.
AI helps:
- Diagnose and treat lung cancer
- Evaluate fibrotic lung diseases
- Interpret pulmonary function tests and manage COPD
- Aids in prioritizing possible therapies
- Predicting the structures of infectious proteins
- Drug discovery
Even with the encouraging results, cautious application of AI in clinical practice is still necessary due to data quality, validation, and ethical issues. [4]
AI & ML together facilitate adaptive treatment planning by continuously learning from patient responses, enabling dynamic adjustments to therapy regimens in real time.

Developments in Biotechnology: Gene Therapy, Stem Cells, and Regenerative Medicine
Gene therapy, leveraging the precision of genetic manipulation, holds the promise of treating and potentially curing a spectrum of genetic disorders by correcting or replacing faulty genes. Stem cell therapies use the regenerative power of versatile cells to repair and regenerate injured lung tissues.
Imagine a time when lung cell-regenerating therapies will be available to patients with chronic respiratory diseases, improving their overall quality of life and lung function. The swift advancement in stem cell research presents great potential for regenerative medicine. It highlights the potential uses of induced pluripotent stem cells (iPSCs) for the treatment of lung and liver diseases, with an emphasis on lung degeneration and Alpha-1 Antitrypsin Deficiency (A1AD). [5]
iPSCs are used to treat diseases like cancer, fibrosis, and tuberculosis in the context of lung degeneration. It is suggested that lung tissue can be restored by transplanting induced pluripotent stem cells (iPSCs) that resemble alveoli and airways. This model is recommended for drug testing, and addressing lung and liver degeneration, it may help improve the treatment of chronic obstructive pulmonary disease (COPD). To address the lack of donor organs, researchers are also looking into 3D bioprinting to create artificial lungs or lung components for transplantation.
Environmental Aspects: Inhaling Clean Air to Promote Respiratory Health
Ensuring a healthier environment for respiratory patients requires investigating green technologies, supporting clean air initiatives, and creating intelligent living environments that reduce respiratory triggers.
Healthcare professionals can use environmental data to personalize recommendations for patients, assisting them in avoiding potential triggers and better managing their respiratory conditions as more advanced sensors and monitoring devices are developed.
Ethical and Regulatory Aspects: Juggling Innovation and Accountability
Addressing ethical and regulatory issues as personalized medicine and AI integration transforms the respiratory care landscape is critical. Nailing the ethical problems posed by these developments requires maintaining transparency in AI algorithms, protecting data privacy, and striking a balance between innovation and patient safety. Building trust between patients and healthcare professionals will require the creation of clear protocols for handling patient data and the development of standardized guidelines for the moral application of AI in respiratory care.
The ethical implications of applying artificial intelligence (AI) to respiratory care demand a thorough analysis of the risks and difficulties involved. Although the merging of technology and healthcare holds great potential for progress, it also raises moral questions that affect medical AI’s dependability and credibility.
Challenges and Barriers in Respiratory Care
Respiratory care, while advancing rapidly, faces a spectrum of challenges and barriers that demand attention and innovative solutions. The challenges encompass a range of issues, such as:
- Algorithmic bias perpetuates health disparities,
- Unstructured medical data affecting algorithm quality,
- Opaque algorithms undermining trust,
- Possible hazards to patient autonomy.
Other challenges include:
- The increasing prevalence of respiratory diseases,
- Increased strain on healthcare systems and resources,
- Keeping up with the technological advancement to avoid integration barriers,
- Affordability and accessibility issues limiting access to healthcare,
- Fragmented healthcare hinders seamless communication.
While regulations concentrate on risk management, algorithm transparency, and data quality, legal frameworks must define accountability. In the quickly changing field of medical AI, international cooperation is crucial for a comprehensive and globally applicable ethical governance system. [6]
Bringing Respiratory Care to Life
There are a lot of fascinating opportunities for respiratory care in the future. AI, biotechnological developments, personalized medicine, and an emphasis on environmental factors can transform how we diagnose and treat respiratory diseases thoroughly. It’s critical to negotiate the ethical, legal, and financial terrain as we enter this uncharted area to ensure that these innovations result in better outcomes and a breath of fresh air for patients in need.
In the future of ICUs, Artificial Intelligence is changing the game. It’s not just a trend; it’s a big step forward for better and more precise care, making critical care even more advanced and effective.
Introducing the Biyovent ICU Ventilator
A revolutionary advancement in respiratory care. What sets Biyovent apart are its exceptional specifications, meticulously crafted to elevate the ventilation process to unprecedented heights. Every aspect of Biyovent has been carefully considered and developed with a holistic approach, ensuring a comprehensive solution for optimal patient care.
In a strategic collaboration with industry leaders Arçelik, Baykar, and Aselsan, Biyovent is not only the result of cutting-edge innovation but is also poised for streamlined mass production. This partnership underscores a commitment to delivering state-of-the-art technology, setting a new benchmark in ventilator design and functionality.
Experience the future of respiratory support with Biyovent ICU Ventilator – where precision meets performance, and healthcare reaches new horizons.
References
[1] Critical Care Therapy and Respiratory Care Section (CCTRCS) | Clinical Center Home Page. (n.d.).: https://www.cc.nih.gov/ccmd/services/cctrcs.html#:~:text=Intensive%20Care%20Unit%3A,to%20most%20critically%20ill%20patient.[2] Honkoop, P., Usmani, O., & Bonini, M. (2022, April 26). The Current and Future Role of Technology in Respiratory Care. Pulmonary Therapy; Adis, Springer Healthcare. https://doi.org/10.1007/s41030-022-00191-y
[3] Hosny, A., Parmar, C., Quackenbush, J., Schwartz, L. H., & Aerts, H. J. (2018, May 17). Artificial intelligence in radiology. Nature Reviews Cancer; Nature Portfolio. https://doi.org/10.1038/s41568-018-0016-5
[4]Applications of AI, Machine Learning, Computational Medicine, and Bioinformatics in Respiratory Pharmacology. (n.d.). Frontiers. https://www.frontiersin.org/research-topics/58254/applications-of-ai-machine-learning-computational-medicine-and-bioinformatics-in-respiratory-pharmacology
[5] Mahla, R. S. (2016, January 1). Stem Cells Applications in Regenerative Medicine and Disease Therapeutics. International Journal of Cell Biology; Hindawi Publishing Corporation. https://doi.org/10.1155/2016/6940283
[6]Zhang, J., & Zhang, Z. (2023, January 13). Ethics and governance of trustworthy medical artificial intelligence. BMC Medical Informatics and Decision Making; BioMed Central. https://doi.org/10.1186/s12911-023-02103-9