Generally, there are two common ways of administering oxygen therapy. One of these is the high-flow device method like air entrainment masks or non-rebreathers. While the other known as low-flow devices use nasal cannula or masks. Many a time, the high-flow nasal cannula are often administered during surgical procedures. Evidence also suggests that this humidified oxygen therapy is safer at a stand-alone surgical IMCU.
Therefore, why is heated and humidified high-flow oxygen (HFNC) necessary for respiratory support? Continue reading to know more.

Understanding Heated and Humidified High-Flow Oxygen Therapy
High-flow oxygen is a respiratory therapy that supplies oxygen at a significantly higher rate. It is a medical device that usually serves as a breathing support for ICU patients. Additionally, it delivers oxygen continuously through a tube inserted into the nostrils. This ventilation supply often aids patient comfort, because they are always humidified and warmed to 37°.
On most occasions, this therapy is mostly used to treat patients experiencing respiratory distress. Also, heated and humidified high-flow oxygen therapy is always provided if standard oxygen therapy isn’t working. Hence, it helps lessen the effort your body must expend on breathing. Apart from reducing respiration effort, it also produces slight positive pressure in the upper airways.
How Does Heated and Humidified High-Flow Oxygen Work?
Unlike conventional low-flow oxygen, HFNC delivers its maximum oxygen rate beyond 30 L/min. Also, this High-flow oxygen isn’t merely a regular nasal cannula but one that’s increased extremely. However, there are some key steps in which heated and humidified high-flow oxygen is produced. Some of these are:
- Oxygen Heat-Up: In most cases, HFNC always heats oxygen to the same temperature as the body. Furthermore, they often provide 37 degrees Celsius of air during inspiration.
- High flow of gas: Additionally, this breathing support works by providing oxygen gas (FiO2) at an elevated inflow rate. It supplies about 1.00% fiO2 at up to 60 liters per minute of flow.
- Provides Humidified Air: Because high-flow therapy is often administered at a high standard, the gas is always humidified. Therefore, inhaled air often contains moisture that is the same as normal air.
- Supplied through Device: Just like any other assisted ventilator, this ventilation support is also supplied via devices. Also, depending on the patient’s fiO2 requirement, the delivering device might be nasal cannulas or masks.

Indication for Using Heated and Humidified High-Flow Oxygen
Sometimes, when standard oxygen therapy fails to improve low oxygen levels, HFNC may be used. In most cases, this heated and humidified high-flow oxygen is often used to support patients experiencing respiratory distress. Nevertheless, some of the breathing issues that always indicate high-flow oxygen usage are as follows:
- Congestive heart failure
- Respiratory distress syndrome (RDS)
- Non-small cell lung cancer (NSCLC)
- Bronchial asthma
- Bronchopneumonia
- Pulmonary edema
- Intensive phase of Chronic obstructive pulmonary disease (COPD)
- Broken ribs and other types of chest trauma
Benefits of Heated and Humidified High Flow Oxygen in Respiratory Care
When compared to traditional oxygen therapy, HFNC offers numerous advantages. They are known as a heated and humidified system that enables easy flow of oxygen. In addition, the fraction of inspired oxygen (fiO2) can be regulated at an extreme inflow rate. Therefore, what are the benefits of high-flow oxygen for patients with respiratory disease?
Accurate Oxygen Distribution
In normal circumstances, the oxygen delivery rates of HFNCs are usually higher than those with traditional nasal cannulas. As a result of this, there is always a limited room air retainment. Besides, it also provides a high amount of oxygen that overcomes the patient’s peak inspiratory flow rate. Therefore, it doesn’t dilute the oxygen wished to give a patient.
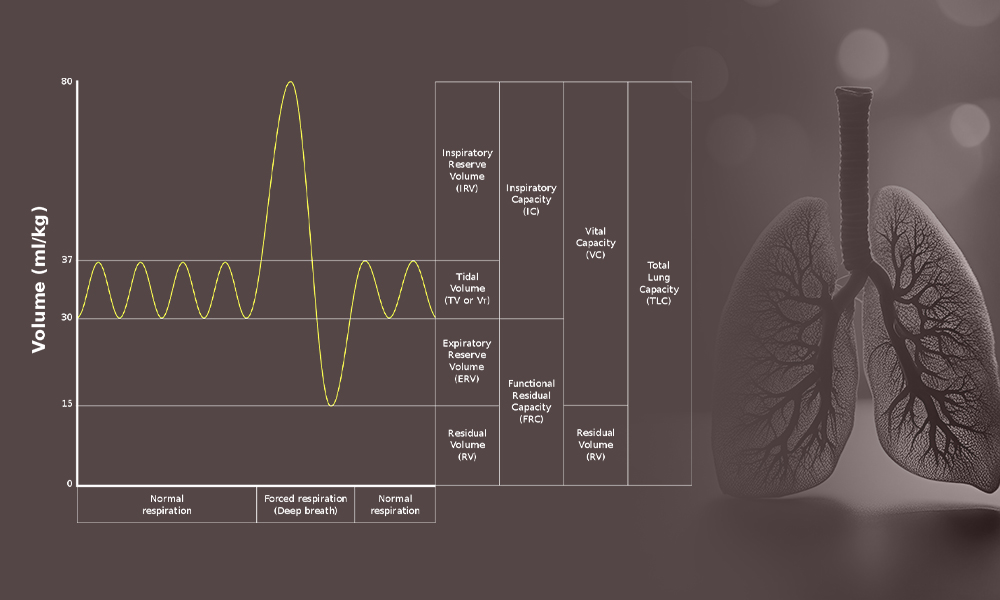
Improves Functional Residual Capacity (FRC)
By supplying a varying amount of positive pressure, high-flow therapy also affects the FRC rate. This is often determined by the placement of manometers at the posterior oropharynx. On most occasions, the readings of this pressure are not always very high during closed-mouth breathing. However, when patients open their mouths, the impact nearly disappears. Additionally, research indicates that the application of HFNC readily results in a 25% improvement in FRC.
Dead space Clearance
Additionally, with heated and humidified high-flow oxygen breathing is usually more efficient. Why? This is because the continuous high oxygen flow often eliminates anatomical dead spaces present in the airways. In addition, the warm, heated air always assists with mucus and foreign particles and also reduces the energy for breathing.

Comparing Heated and Humidified High-Flow Oxygen to Traditional Oxygen Therapy
When comparing high-flow oxygen to traditional oxygen, several differences and similarities can be extracted. However, some following points indicate the similarities of both systems.
- Most of the time, both devices supply FiO2 at a variable concentration
- They also serve as respiratory support
- Neither traditional oxygen nor HFNC are delivered in the invasive mode
- In most cases, they are simple to administer and easily adjustable
- Either of the two systems can be used effectively in similar clinical conditions e.g. COPD cases, acute respiratory failure etc.
Although, heated and humidified high-flow oxygen provides some similar functions to traditional oxygen. Hence, this high-flow device also has some specialty when compared to the low-flow. Some of these significant features are:
- The ability to provide oxygen gas at a very high rate that ranges between 30 to 60 L/min
- Capacity to actively moisturize inflow air
- Provision warm oxygen that complies with body temperature
- Prevent airway problems and complications by maintaining and clearing respiratory dead spaces
- HFNC is also more effective at improving oxygenation, especially in hypoxemic patients.
Considerations for Implementing Heated and Humidified High-Flow Oxygen
Normally, heated and humidified high-flow oxygen is easy to use. Nonetheless, some integral factors must be considered while implementing this device. Hence, I would like to give you some basic “DEDEVUS” processes that must be considered while using HFNC.
- Determine your patient condition and device compliance rate
- Ensure a proper setting of the system: You must make sure the high-flow device is in good form. Additionally, thighs like the flow rate, FiO2 level, filter, battery, and ventilation slot should be examined thoroughly.
- Don’t place a patient on high-flow oxygen immediately after the device is turned on.
- Examine your oxygenation channels: It’s very important to verify the O2 tube connection and adjust flow to prevent FiO2 delay and regulate the flowmeter. In addition, ensure to set your internal alarm menu and avoid smoking.
- Verify humidification supply: Things like sterile water, plastic bags, and caps should be checked thoroughly. Also, the water bag must not be empty and the permeable circuit must be monitored at every interval.
- Use the appropriate tube and cannula with the correct placement
- Set alarm
Future Directions and Innovations in Heated and Humidified High-Flow Oxygen Technology
In the modern world, almost every aspect of life is gradually evolving. Some of these have led to several innovative improvements in the medical world and assisted ventilation to be precise. Hence, heated and humidified high-flow oxygen isn’t left aside. Also, most scientists believe they are one of the best and most dynamic mechanical ventilation systems. Therefore what are high-flow oxygen future trends?
Be informed that several innovative directions of HFNC are yet to be seen. However, some of these potential features and trends, such as precise delivery, flexibility, patient compliance, personalized treatment, etc are expected to emerge soon.
Biosys Biomedical: A Reliable Respiratory Support
Heated and humidified high-flow oxygen therapy is a modern method that provides a great deal of warmed and moisturized oxygen. It is a special device with significant advantages that plays a key role in patient outcomes. Additionally, this system is a breathing support that requires proper examination before implementation as it differs from traditional oxygen therapy. Above all, it’s also a ventilation system with diverse emerging future directions.
However, high-flow oxygen is a medical therapy that requires professionalism. So, if you are looking for a reliable source of respiratory support, you can reach out to Biosys Biomedical today. With no more ado, schedule an appointment for effective HFNC support today!
References
https://tsaco.bmj.com/content/3/1/e000179
https://www.accjournal.org/journal/view.php?doi=10.4266/acc.2021.01571
https://www.svhlunghealth.com.au/procedures/procedures-treatments/high-flow-oxygen-therapy
https://rebelem.com/high-flow-nasal-cannula-hfnc-part-1-how-it-works/
https://ejb.springeropen.com/articles/10.4103/1687-8426.211399
https://clinmedjournals.org/articles/ijccem/international-journal-of-critical-care-and-emergency-medicine-ijccem-4-048.php?jid=ijccem#:~:text=
https://www.biosysmed.com/innovative-approaches-high-flow-oxygen-therapy-in-the-icu/