Intraoperative neuromonitoring (IONM) is a technique aimed at monitoring and protecting the nervous system, particularly nerves and the spinal cord, during surgery. It is primarily used in surgeries where there is a high risk of damage to the nerves or nervous system.
Why is intraoperative neuromonitoring important?
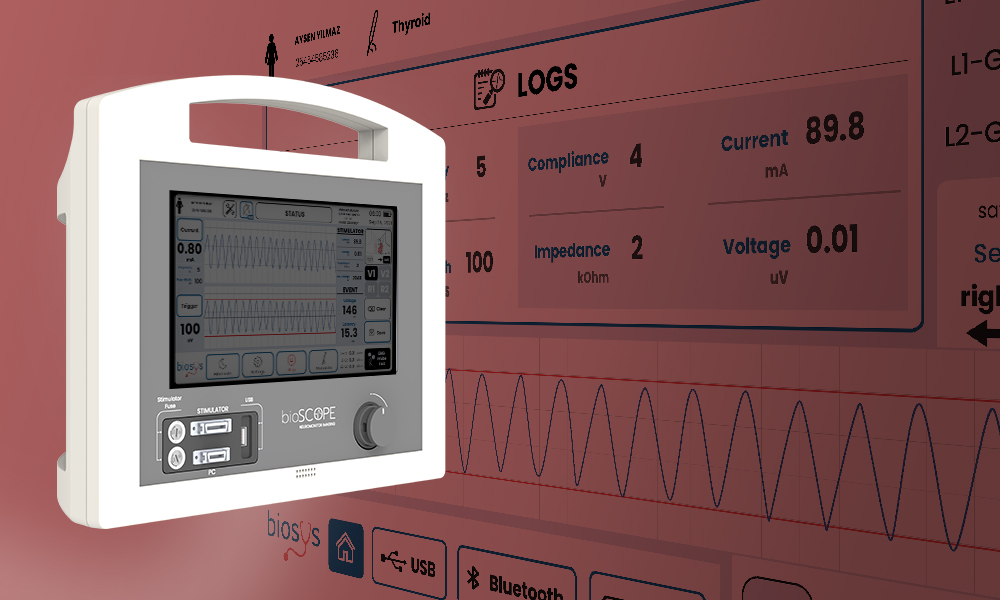
Neuromonitor reduces the risk of permanent damage by enabling real-time monitoring of nerve functions during surgeries that may pose a threat to the nervous system. Neuromonitoring devices facilitate the surgeon’s work by identifying potential damage to nerves in procedures involving the brain, spinal cord, and nerve roots, thus providing the capability to monitor and protect nerve tissues. For instance, the use of IONM in brain tumor and spinal surgeries helps prevent complications such as sensory loss or paralysis.
Additionally, nerve monitoring can positively impact the postoperative recovery process. By minimizing permanent losses in motor and sensory functions, IONM contributes to an improved quality of life for the patient.
The Benefits of Neuromonitoring on Patient Outcomes
Neuromonitoring offers significant health and safety benefits by enabling real-time monitoring of patients’ nervous systems during surgical procedures. Neuromonitoring devices are commonly used in brain, spinal, vascular, and thyroid surgeries, helping to minimize surgical risks by preventing damage to nerve tissues.
Surgeries Where Neuromonitoring Devices Are Commonly Used
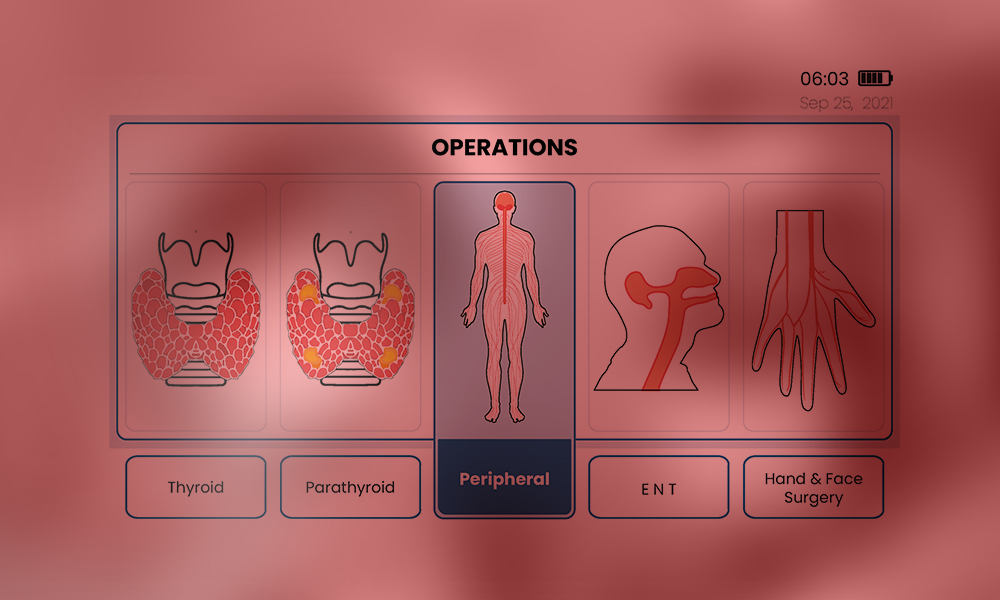
- Thyroid & Parathyroid Surgeries: Neuromonitoring is a crucial technology in preventing nerve injuries, particularly focusing on protecting the nerves that control the vocal cords. These nerves are located very close to the thyroid gland, and any damage to them during surgery can lead to complications such as hoarseness or even loss of voice. IONM allows the surgeon to work with precision by monitoring these nerves, thereby reducing the risk of nerve injury. The use of IONM is especially beneficial in recurrent goiter and complex thyroid surgeries, as it helps minimize issues like hoarseness and accelerates the postoperative recovery process.
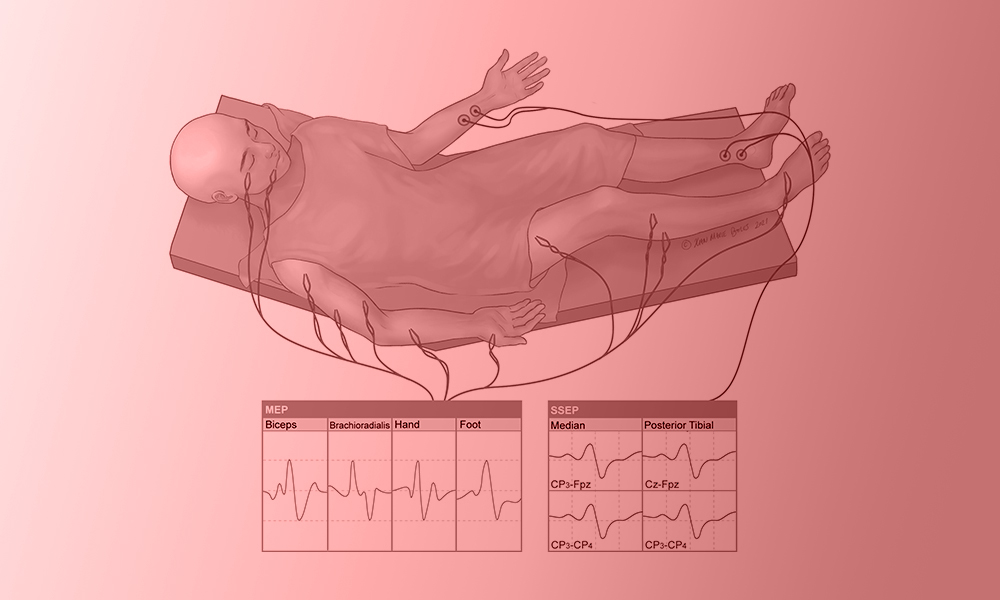
- Spinal Surgeries: In spinal surgery, IONM plays an essential role in protecting nerve roots, the spinal cord, and neural pathways. Spinal surgeries carry a high risk of nerve or spinal cord injury, necessitating a monitoring system to help the surgeon perform the procedure safely.
- Brain Surgeries: Brain surgeries are performed in areas containing delicate neural tissues, and the use of neuromonitoring devices helps protect neurological structures by monitoring the brain and nervous system in real time.
- Peripheral Nerve Surgeries: Peripheral nerves transmit sensory and motor signals to specific parts of the body. Damage to these nerves can lead to complications such as loss of muscle control, sensory disturbances, or pain. In peripheral nerve surgeries, neuromonitoring devices provide the surgeon with real-time information to prevent nerve damage, ensuring effective nerve monitoring.
- Vascular Surgeries: Neuromonitoring is employed when nerves are located close to vascular structures and there is a risk of nerve injury. In surgeries on major blood vessels, protecting nerves around these structures is critical. For example, procedures like carotid artery surgery or aortic aneurysm repairs carry a high risk of nerve damage, making neuromonitoring essential for safeguarding these nerves.
FAQs
1. What are the risks of not using neuromonitoring in certain surgeries?
In surgeries where neuromonitoring is not used, the risk of nerve damage increases, which can lead to temporary or permanent neurological complications. When nerves are unprotected, patients may experience permanent paralysis, sensory loss, or other motor and sensory impairments.
2. Who performs and monitors IONM during surgery?
The neuromonitoring setup is managed by a neuromonitoring specialist, and it is used collaboratively by the surgeon and anesthesiologist throughout the surgery.
3. Is intraoperative neuromonitoring safe for all patients?
While IONM is generally considered a safe technique, the electrodes in contact with the skin can cause allergic reactions or skin irritation in some patients. Temporary side effects such as localized pain or muscle spasms may also occur in certain cases.
References:
- Skinner, S.A. ∙ Cohen, B.A. ∙ Morledge, D.E. Practice guidelines for the supervising professional: intraoperative neurophysiological monitoring. J Clin Monit Comput. 2014; 28:103-111
- R Malik, D Linos. Intraoperative neuromonitoring in thyroid surgery: a systematic review. World journal of surgery, 2016 – Springer
- Wong, Andrew K., et al. “Intraoperative neuromonitoring.” Neurologic Clinics 40.2 (2022): 375-389.
- Shils, Jay L., and Tod B. Sloan. “Intraoperative neuromonitoring.” International anesthesiology clinics 53.1 (2015): 53-73.