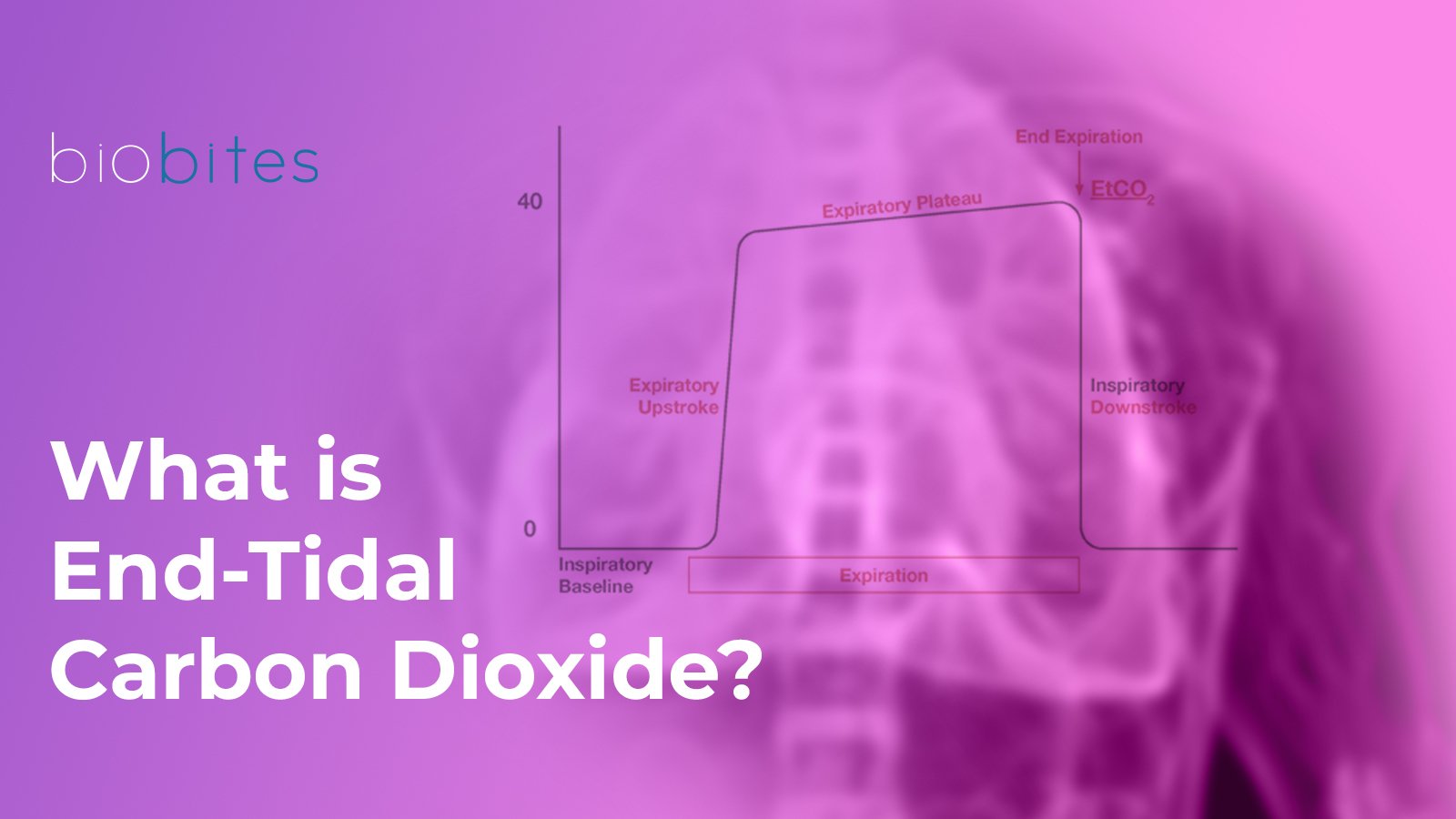
EtCO₂ (End-Tidal Carbon Dioxide) refers to the measurement of the carbon dioxide concentration in exhaled air at the end of expiration. It is typically expressed in millimeters of mercury (mmHg) and measured using a capnography device. It provides critical insights into the respiratory system, cardiac circulation, and metabolism.
At the end of the respiratory cycle, during exhalation, EtCO₂ represents the peak concentration of carbon dioxide (CO₂) in the exhaled gas. This value forms the basis of EtCO₂ monitoring. By reflecting the interaction between the respiratory system, circulation, and metabolism, it plays a crucial role in assessing the patient’s overall condition.
Normal EtCO₂ Values
The normal EtCO₂ level typically ranges between 35 and 45 mmHg.
- Low EtCO₂: May indicate conditions such as hyperventilation, low cardiac output, or pulmonary embolism.
- High EtCO₂: May suggest hypoventilation, excessive metabolic activity, or inadequate ventilator settings.
Monitoring EtCO₂ levels with mechanical ventilators plays a critical role in evaluating a patient’s respiratory status and the effectiveness of ventilation. This monitoring is performed using capnography devices, which are often integrated into the ventilator system.
EtCO₂ Monitoring Methods
- Mainstream Capnography
- How It Works: The sensor is placed between the endotracheal or tracheostomy tube and the breathing circuit. The patient’s exhaled air passes directly through the sensor, and CO₂ concentration is measured in real-time.
- Advantages: Provides instantaneous and accurate measurements with minimal delay during exhalation.
- Disadvantages: The sensor’s weight and heat may cause discomfort, particularly for small children or frail patients.
- Sidestream Capnography
- How It Works: A small gas sample is drawn from the breathing circuit and delivered to the analyzer within the device. This method can also be used for non-intubated patients.
- Advantages: Compatible with various breathing circuits and suitable for patients who do not require intubation.
- Disadvantages: Condensation may accumulate in the sampling line, potentially affecting measurement accuracy.
Ventilation Efficiency Through EtCO₂ Monitoring
EtCO₂ monitoring is a direct method to evaluate ventilation efficiency. It demonstrates how effectively the respiratory system eliminates carbon dioxide (CO₂) and assesses the efficiency of CO₂ removal produced through metabolic processes via ventilation. Ventilation efficiency is evaluated in various clinical conditions using EtCO₂ levels and capnogram analyses.
- Hypoventilation (Decreased Ventilation):
- EtCO₂ Level: Increased (typically > 45 mmHg).
- Cause: Inadequate elimination of CO₂ by the lungs.
- Clinical Conditions: Respiratory depression, sedation, neuromuscular blockade, obesity hypoventilation syndrome.
- Effect: Elevated EtCO₂ levels indicate the need to enhance ventilation.
- Hyperventilation (Increased Ventilation):
- EtCO₂ Level: Decreased (typically < 35 mmHg).
- Cause: Excessive elimination of CO₂.
- Clinical Conditions: Anxiety, pain, response to hypoxia, compensatory mechanisms.
- Effect: A reduction in ventilation rate or tidal volume may be necessary.
- Increased Alveolar Dead Space:
- EtCO₂ Level: Decreased, but arterial CO₂ (PaCO₂) remains elevated.
- Cause: Reduced pulmonary perfusion or ventilation-perfusion (V/Q) mismatch.
- Clinical Conditions: Pulmonary embolism, low cardiac output, shock.
- Effect: The difference between EtCO₂ and PaCO₂ increases (EtCO₂-PaCO₂ gradient).
- Circulatory Failure:
- EtCO₂ Level: Decreased.
- Cause: Reduced cardiac output decreases the amount of CO₂ delivered to the alveoli.
- Clinical Conditions: Cardiac arrest, low-perfusion shock.
- Effect: Used to monitor the effectiveness of CPR; an increase in EtCO₂ indicates the restoration of circulation.
FAQs
- What is the normal EtCO₂ value?
The normal range is between 35-45 mmHg. - What does low EtCO₂ mean?
Low EtCO₂ refers to a condition where the carbon dioxide level in exhaled air is below normal. This may indicate issues related to ventilation, perfusion, or metabolism. EtCO₂ levels below 35 mmHg are typically referred to as hypocapnia. - What are the causes of low EtCO₂ on a ventilator?
Low EtCO₂ is commonly caused by factors such as hyperventilation, hypoperfusion, airway issues, or decreased metabolic activity.
References
- Aminiahidashti, Hamed, et al. “Applications of end-tidal carbon dioxide (ETCO2) monitoring in emergency department; a narrative review.” Emergency 6.1 (2018).
- Trilĺo, Giulio, Martin von Planta, and Fulvio Kette. “ETCO2 monitoring during low flow states: clinical aims and limits.” Resuscitation 27.1 (1994): 1-8.
- Miner, James R., William Heegaard, and David Plummer. “End‐tidal carbon dioxide monitoring during procedural sedation.” Academic Emergency Medicine 9.4 (2002): 275-280.
- Paiva, Edison F., James H. Paxton, and Brian J. O’Neil. “The use of end-tidal carbon dioxide (ETCO2) measurement to guide management of cardiac arrest: a systematic review.” Resuscitation 123 (2018): 1-7.